Full Length Research Paper
ABSTRACT
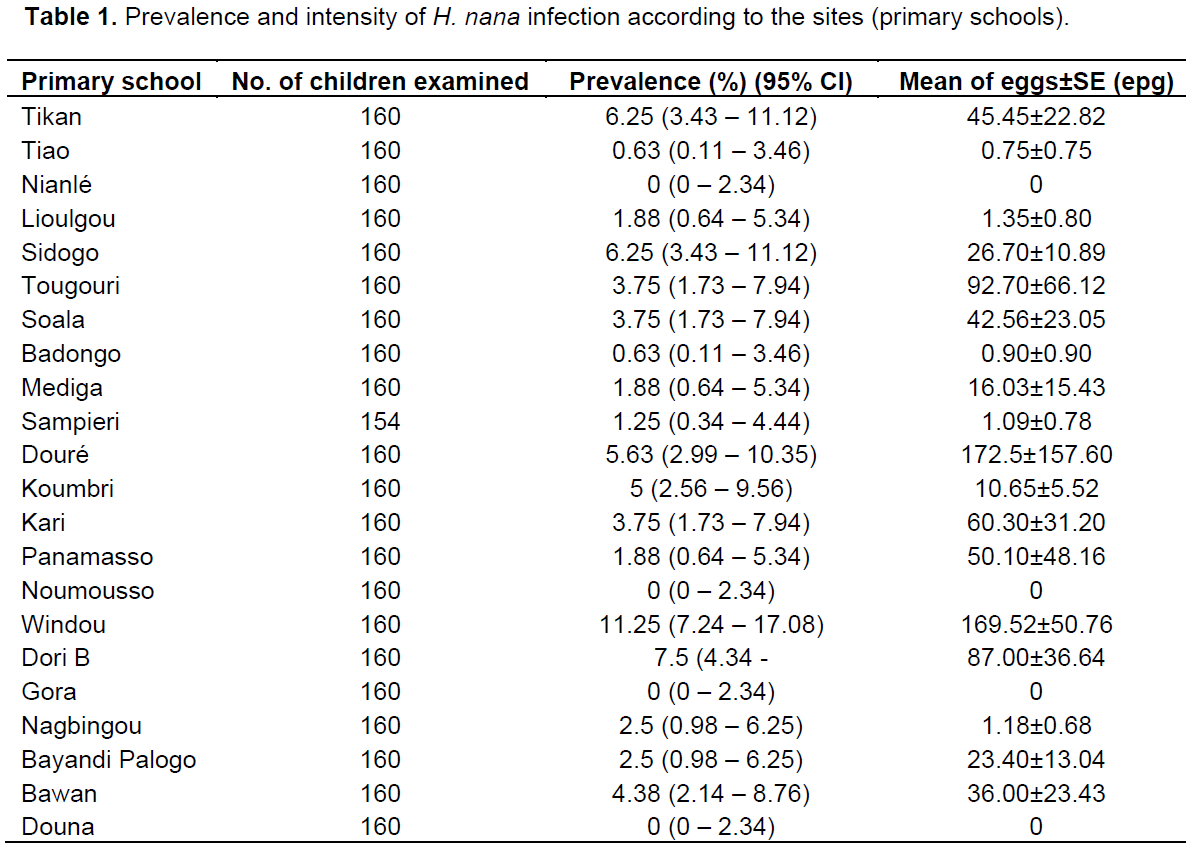
This cross-sectional descriptive study estimated the prevalence of Hymenolepis nana infection in primary school children living in Burkina Faso. A parasitological survey was conducted in 2013 in 22 primary schools located in eleven regions of Burkina Faso. Kato-Katz method was used as a technique to detect the H. nana eggs. The prevalence and intensity of the infection were determined by estimating the means of H. nana eggs per gram of faeces (epg). 3514 school children from 7 to 11 years old have been investigated. The overall prevalence of H. nana was 3.22%. It varied from 0 to 11.25% among the primary schools (p<0.001). The difference was not significant according to gender (p=0.963) and the children aged 8 and 9 years were more infected (p=0.021). The highest mean intensity of eggs was 162 epg according the primary schools. The distribution of H. nana in Burkina Faso was determined. The prevalence of H. nana was low in the different primary schools.
Key words: Prevalence, Hymenolepis nana, school children, Burkina Faso.
INTRODUCTION
MATERIALS AND METHODS
RESULTS
DISCUSSION
CONCLUSION
CONFLICT OF INTERESTS
ACKNOWLEDGEMENTS
REFERENCES
|
Al-Shammari S, Khoja T, El-Khwasky F Gad A (2001). Intestinal parasitic diseases in Riyadh, Saudi Arabia: prevalence, socio demographic and environmental asoociates. Trop. Med. Int. Health 6:184-189. |
|
|
Becker SL, Lohourignon LK, Speich B, Rinaldi L, Knopp S, N'Goran EK, Gringoli G, Utzinger J (2011). Comparaison the flotac-400 dual technique and formalin-ether concentration technique for diagnosis of Human intestinal protozon infection. J. clin. Microbiol. 49(6):2183-2190. |
|
|
Cissé M, Coulibaly SO, Guiguemdé TR (2011). Aspects épidemiologiques des parasitoses intestinales rapportées aux Burkina Faso de 1997 à 2007. Med. Trop. 71:257-260. |
|
|
Dianou D, Poda JN, Savadogo LG, Sorgho H, Wango SP, Sondo B (2004). Parasitoses intestinales dans la zone du complexe hydroagricole du Sourou au Burkina Faso. VertigO (Rev Sci Env), 5p. |
|
|
Farid Z, EL-Masry A, Wallace CK (1984). Treatment of Hymenolepis nana with single oral dose of praziquantel. Trans. R. Soc. Trop. Med. Hyg. 78:280-281. |
|
|
Gelaw A, Anagaw B, Nigussie B, Silesh B, Yirga A, Alem M, Endris M, Gelaw B (2013). Prevalence of intestinal parasitic infections and risk factors among schoolchildren at the University of Gondar Community School, Northwest Ethiopia: a cross-sectional study. BMC public health. 13(7):304. |
|
|
Huda-Thaher A (2012). Prevalence of Hymenolepis nana infections in Abu Ghraib City (Baghdad/Iraq).The Iraqi Post graduate Med. J. 11(4):581-584. |
|
|
Katz N, Chaves A, Pellegrino J (1972). A simple device for quantitative stool thicks mear technique in schistosomiasis mansoni. Revista do Instituto de Medicina Tropical de Sao Paulo, 14:397-400. |
|
|
King CH (2010). Cestodes (Tapeworms). In Mandell GL, Benett JE, Dolin R, Editors Mandell Douglas and Benett's principles and pratice of infectious disease. 7 th edition. Philadephia: Churchull Livingstone. Elsevier. 3609-3610. |
|
|
Knopp S, Rinaldi L, Khamis IS, Stothard JR, Rollinson D, Maurelli DM, Steinmann P, Marti H, Cringoli G, Utzinger J (2009). A single FLOTAC is more sensitive than triplicate Kato-Katz for the diagnosis of low-intensity soil-transmitted helminth infections. Trans. Royal Soc. Tropical Med. Hyg. 103:347-354. |
|
|
Kpoda NW, Oueda A, Some SYC, Cisse G, Maïga AH, Kabre GB (2015). Physicochemical and parasitological quality of vegetables irrigation water in Ouagadougou city, Burkina –Faso. Afr. J. Microbiol. Res. 95(5):307-317. |
|
|
Kremer M, et Molet B (1975). Interêt de la technique de Kato en coprologie parasitaire. Anna. Soc. Belge Med. Trop. 55(5):427-430. |
|
|
Magalhaes Soares JR, Fançony C, Gamboa D, Langa AJ, Sousa-Figueiredo JC, Clements ACA, Nery SV (2013). Extanding helminths control beyond STH and schistosomiaisis: The case of Human Hymenolepiasis. Plos Negl. Trop. Dis. 7(10). |
|
|
Malheiros AF, Mathews PD, Lemos LMS, Braga GB, Shaw JJ (2014). Prevalence of Hymenolepis nana in indigenous Tapiré Ethnic group from the Brazilian Amazon. Am. J. Biomed. Res. 2(2):16-18. |
|
|
Martinez-Barbabosa I, Gutierrez-Cardenas EM, Gaona E, Shea M (2010). The prevalence of Hymenolepis nana in schoolchildren in a bicultural community. Rev. Biomed. 21:21-27. |
|
|
Mason PRP (1994). Epidemiology of Hymenolepis nana infection in primary schoolchildren in urban and rural communities in Zimbabwe. J. Parasitol. 80:245-250. |
|
|
Matthys B, Bobieva M, Karimova G, Mengliboeva Z, Jean-Richard V, Hoimnazarova M, Kurbonova M, Lohourignon LK, Utzinger J, Wyss K (2011). Prevalence and risk factors of helminths and intestinal protozoa infections among children from primary schools in western Tajikistan. Parasit Vectors, 4(1):195. |
|
|
Mirdha BR, Samantray JC (2002). Hymenolepis nana : A common cause of pediatric diarrhoea in urban Sleem dwellers in India. J. Tropi. Pediatr. 48:330- 334. |
|
|
Mohammad MA, Hegazi MA (2007). Intestinal permeability in Hymenolepis nana as reflected by non invasive lactulosa/manitol dual permeability test an dits impaction on nutritional parameters of patients. J. Egypt Soc. Parasitol. 37:877-891. |
|
|
Montresor A, Crompton DWT, Gyorkos TW, Savioli L (2004). Lutte contre les helminthiases chez les enfants d'âge scolaire: Guide à l'intention des responsables des programmes de lutte. Organisation Mondiale de la Santé. Génève. ISBN 92 4 254556 2. 91p. |
|
|
Ouermi D, Karou DS, Ouattara I, Gnoula C, Pietra V, Moret R, Pignatelli S, Nikiema JB, Simpore J (2012). Prévalence des parasites intestinaux de 1991 à 2010 au centre médical Saint-Camille de Ouagadougou (Burkina Faso). Med. Sante Trop. 22:40-44. |
|
|
Poda JN, Mwanga J, Dianou D, Garba A, Ouédraogo FC, Zongo D, Sondo KB (2006). Les parasitoses qui minent les nouveaux pôles de développement au Burkina Faso : cas des schistosomoses et des géo-helminthes dans le complexe Hydro-agricole du Sourou. VertigO, Vol. 7, N°2: 1-7. |
|
|
Poda JN (2007). Les maladies liées à l'eau dans le bassin de la Volta : état des lieux et perspectives. Volta Basin Focal Project Report No 4. IRD, Montpellier, France, and CPWF, Colombo, Sri Lanka, 87p. |
|
|
Rim HJ, Parck CY, Lee JS, Joo KH, Lyu KS (1978). Therapeutic effects of praziquantel (Embay 8440) against Hymenolepis nana infection. The Korean J. Parasitol. 16(2):82-87. |
|
|
Sharif M. (2015). Prevalence of intestinal parasite among food handlers of Sari Northern Iran. Rev. Inst. Med. Trop. Sao Paulo 57(2):139-144. |
|
|
Sangaré I, Bamba S, Cissé M, Zida A, Bamogo R, Sirima C, Yaméogo BK, Sanou R, Drabo F, Dabiré RK, Guiguemdé RT (2015). Prevalence of intestinal opportunistic parasites infections in the University hospital of Bobo-Dioulasso, Burkina Faso. Infect. Dis. Poverty 4(32):6. DOI 10.1186/s40249-015-0065-x |
|
|
Tadesse G (2005). The prevalence of intestinal helminthic infections and associates risk factors among schoolchildren in Babile town eartern Ethiopia. Ethop. J. Health Dev. 19:140-147. |
|
|
Zida A, Sangaré I, Bamba S, Sombié I, Traoré LK, Coulibaly SO, Menan H, Guiguemdé TR (2014). Prévalence du parasitisme intestinal en milieu carcéral à Ouagadougou (Burkina Faso). Médecine et Santé Tropicale, 24:383-387. |
|
|
Zongo I, Drabo MK, Guiguemde TR et Ouedraogo JB (2006). Parasitoses intestinales en milieu scolaire dans la ville de Bobo-Dioulasso. Sci. Technol. 29(1,2):57-64. |
|
Copyright © 2024 Author(s) retain the copyright of this article.
This article is published under the terms of the Creative Commons Attribution License 4.0