ABSTRACT
Various factors had been related with sputum conversion in tuberculosis patients, which constituted an essential indicator of the effectiveness of treatment and the infectivity of patients. The study evaluates the factors related with smear sputum conversion in pulmonary tuberculosis. A retrospective cohort study of newly diagnosed pulmonary tuberculosis was performed from January 2013 to September 2016 in Cuban Hospital (Qatar). The data collected includes: demographics, clinical, laboratory test and chest X ray. The Kaplan Meier method was used to calculate the survival time to sputum conversion. The log-rank or Wilcoxon tests and Cox regression was used to identify the variable related with sputum conversion. In 323 patients, the median time of sputum conversion was 23 days, with sputum conversion at 2 months of treatment in 82.1% of patients. In older patients (39-86 years old), the probability of conversion was 31% lower when compared with patients 16-24 years old (RR 0.69, 95% CI, 0.52-0.90). The low figures of serum albumin (0.71, 0.56-0.90) and absolute lymphocyte count (0.64, 0.48-0.85) were associated with a decreased probability of sputum conversion, and the lower probabilities of conversion were found with the increased number of bacilli; among 1501 to 2000 (0.39, 0.23-0.66), and 2001 to 5000 (0.40, 0.28-0.58). The factors associated with delayed smear sputum conversion in tuberculosis patients were identified. Additional studies are required to evaluate the influence of nutritional status on TB diagnosis and the poor glycemic control in conversion times as well as interventions to modify these factors to improve the patient outcomes.
Key words: Infectious tuberculosis, sputum conversion, factors associated, Qatar.
The incidence of tuberculosis (TB) in Qatar is related to the expatriate population, mainly from countries with high TB burden (Nepal, India, Bangladesh Philippines), with few cases from the native population (Hamad Medical Corporation (HMC), 2012). The national program of TB guides the provision of care in line with the national and regional priority for its prevention and control (Hamad Medical Corporation (HMC), 2011). The sputum smear and culture conversion constitute an essential indicator of the effectiveness of treatment and the infectivity of patients. The conversion time has been related with multiple factors including nutritional factors such as anemia, magnesium level, and body mass index (Bhargava et al., 2013; Putri et al., 2014; Agrawal, 2017), history of diabetes mellitus and poor metabolic control (Mi et al., 2013; Nakamura et al., 2014; Sharif, 2015), bacillary load in the diagnosis (D'Souza et al., 2018; Kanda et al., 2015; Gunda, 2017), diagnosis delay and radiological lesions suggestive of extensive damage or cavitation (Mi et al., 2013; Nakamura et al., 2014; Unsematham and Kateruttanakul, 2013; Visser et al., 2012) and drug resistance (Kim et al., 2016; Holtz et al., 2006; Kurbatova et al., 2012). A previously published paper identifies the bacillary load in the diagnosis as the main factor related with sputum conversion in patients attended to in a community hospital in Qatar, but the study is limited by the number of patients studied (64 patients) (Guanche et al., 2016). More than 700 patients are annually reported in the country (WHO, 2017). The National Program of TB recommends the provision of free healthcare services to all TB patients regardless of nationally, inclusive of diagnosis, treatment and follow-up. Patients with infectious TB are admitted to hospital facilities until 2 consecutive negative results of sputum smear are obtained (Hamad Medical Corporation (HMC), 2011). After hospital discharge, the patients are followed in an infectious disease clinic until completion of treatment. The Cuban Hospital provide secondary healthcare services to a community located in Western Qatar and receive patients with TB from local areas or transfer from other facilities due to beds crisis. This study was conducted to evaluate the factors related to smear sputum conversion in patients with pulmonary TB attended to in a community hospital in Western Qatar.
A retrospective cohort study was performed. All patients admitted to the Cuban Hospital (Qatar) newly diagnosed of pulmonary TB and positive smear sputum, from January 2013 to September 2016, were studied. All data were collected from patients' medical records. The variables were: age, sex, delay in diagnosis (time between first symptoms and diagnosis), active smoking, history of previous TB and diabetes mellitus, and the maximum number of bacilli found at the time of the diagnosis. Laboratory results were classified as "normal" or "low" according to the following reference values: Absolute lymphocyte count 1000-3000 / μl; hemoglobin, men 13 - 17 g/L, women 12 - 15 g/L; platelet count 150 - 400 × 103; serum albumin, male 32 - 47 g/L, female 29 - 42 g/L; total proteins 60-80 g/L,; serum creatinine, men 71 - 123 μmol/L, women 53 - 97 μmol/L and serum iron, men 8.1 - 28.6 μmol / L, and women 5.4 - 28.6 μmol/L. The presence of bilateral lesions, pleural effusion, consolidation and cavities were identified with chest X-ray. The body mass index was calculated from the first data recorded at admission, using the formula weight (Kg)) divided by size (m2). All patients were treated with a standard regimen of rifampicin, isoniazid, pyrazinamide, and ethambutol, except for patients who had resistance to rifampicin, which was identified through Gene Xpert PCR/RIF. The date of onset of treatment and the dates of sputum collection were recorded. The sputum conversion was considered when two consecutive sputum smears became negative. The date of the first negative result was considered the date of sputum conversion. The time period between initiation of treatment and sputum conversion was the primary response variable (SputumConversion Time). All the information was collected from the patient´s files. The study was approved by the hospital board. This retrospective study meets the criteria for exemption from ethics review.
Statistics
All the information was processed in SPSS version 22.0. The initial descriptions of the demographic and clinical characteristics were calculated by the absolute and relative frequencies (percentages). The Kaplan Meier method was used to calculate the survival time to sputum conversion. The starting date of the TB treatment was considered the beginning of the follow-up in each subject. The date of conversion was taken as the event or terminal condition. Individuals were followed periodically, by performing sputum tests every 2 weeks, and there were no incomplete follow-up times. Initially, to identify the variables related to sputum conversion, the survival curves obtained were compared between the categories of the variables using log-rank or Wilcoxon tests, depending on the existence of proportionality between them. Subsequently, to evaluate the pure effect of each of the variables in the sputum conversion time, the Cox regression was used. The model included the following variables: Age, history of diabetes mellitus, the maximum number of bacilli, hemoglobin, total serum protein, serum albumin, absolute lymphocyte counts, serum iron, and pulmonary cavitation, as independent variables, and the time to sputum conversion, as the dependent variable. For all hypothesis tests that were performed, a significance level a = 0.05 was set.
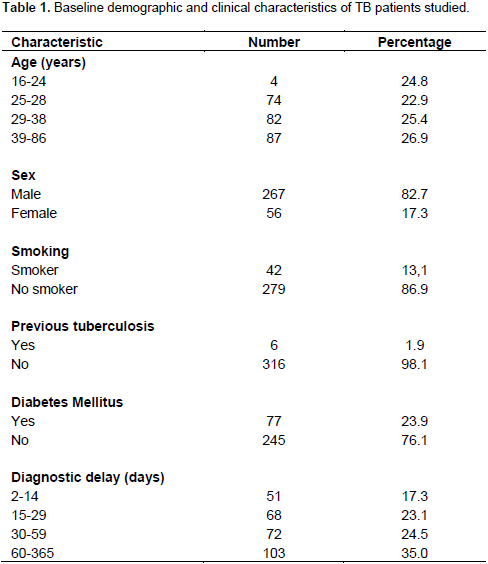
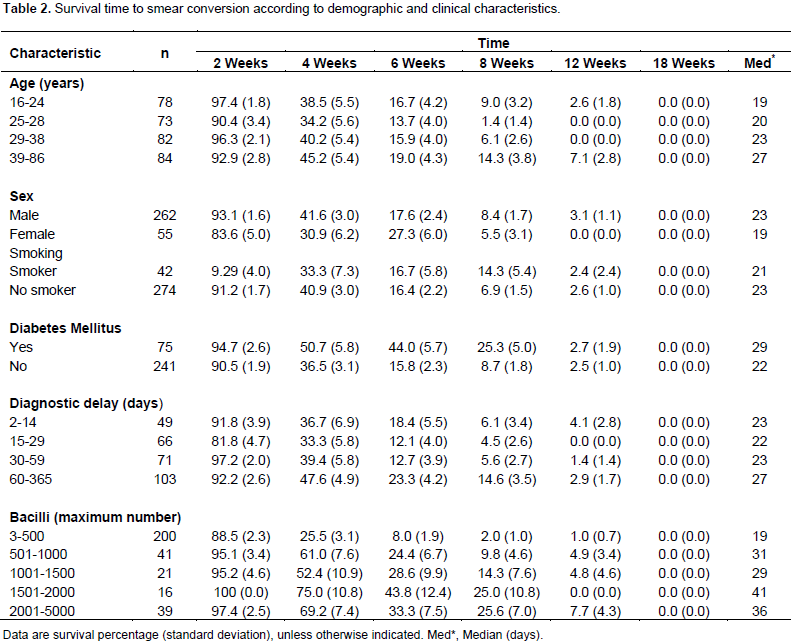
From January 2013 to September 2016, a total of 323 patients with a diagnosis of pulmonary TB were admitted. Table 1 shows the demographic and clinical characteristics of these patients. As it can be seen, significant percentages (73.1%) were below 39 years of age. The mean age was 32.8 years (standard deviation 11.5 years). Patients were predominantly male (82.7%), non-smokers (86.9%) and without previous history of pulmonary TB (98.1%). In addition, 77 patients (23.9%) had diabetes mellitus and 59.5% had 30 days or more of delay in diagnosis. Figure 1 show the survival time to patient sputum conversion, estimated by the Kaplan Meier method. The median time was 23 days (minimum 3 days; maximum 117 days), with sputum conversion at 2 months of treatment in 82.1% of patients. When the survival curves were compared to the sputum conversion between the categories of demographic and clinical variables, statistically significant differences were found for age (p = 0.03), the presence of diabetes mellitus (p = 0.03) and the maximum number of bacilli (p = 0.00). For ages, the differences were in the group of 39-86 years of age compared with patients in the 16-24 years of age group (p = 0.03) and 25-28 years of age group (p = 0.01). For the number of bacilli, the differences were found when comparing the category of smaller number of bacilli (3-500 bacilli), with the remaining categories (p = 0.00 in all cases).

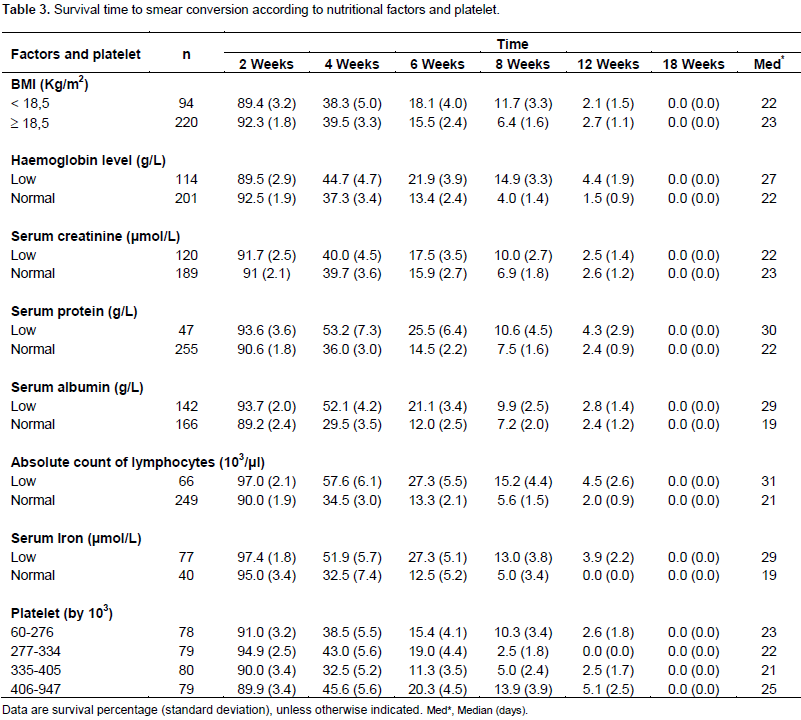
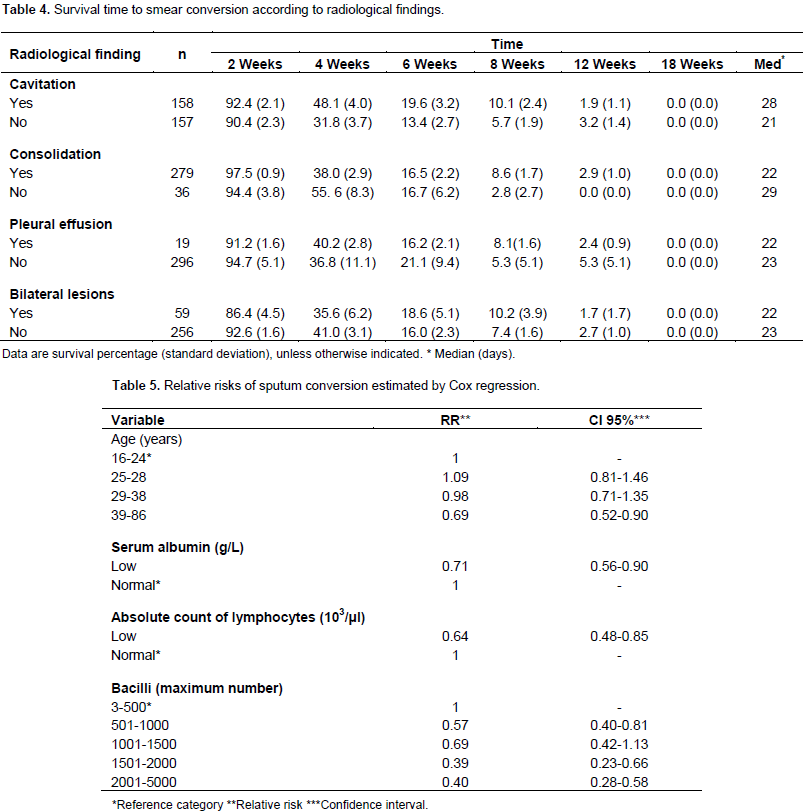
It can be seen from Table 2 that the median bacilli survival time for patients 39-86 years of age (27 days) was higher when compared to patients 25-28 years old (20 days) and patients 16-24 years of age (median of 19 days). The survival time was higher for diabetic patients (29 days vs. 22 days for non-diabetic patients), and lower for patients with 3-500 bacilli (19 days), when compared with the remaining groups of patients according to the maximum bacilli number; the group with the lowest median survival time was observed in patients with 1001-1500 bacilli at the time of diagnosis (29 days). Among the categories of the variables body mass index (p = 0.92), serum creatinine (p = 0.77) and platelet count (p = 0.26), there were no statistically significant differences when comparing survival curves up to the sputum conversion (Table 3). For the other nutritional indicators, statistically significant differences were found when comparing the survival curves between categories (p <0.05 in all comparisons). The differences between medians of survival time were higher when the nutritional factor was low. The greatest differences were found for serum albumin, absolute lymphocyte counts, and serum iron. In the first and third indicator, when the nutritional indicator was normal, the median survival time was 19 and 29 days when the figures were low. In relation to the lymphocyte count, there was a median survival time of 21 days in patients with normal figures and 31 days when the figures were low. Regarding the radiological findings, statistically significant differences were found when comparing the survival curves for the variable cavitation (p = 0.01). It can be seen that among the median of the survival times for the categories of the consolidation, the differences were similar to those found between the categories of the cavitation, without statistically significant differences (p = 0.32).
Among the median survival times of the categories for the remaining variables, the differences were much smaller (Table 4). Table 5 shows the relative risks of sputum conversion estimated by Cox regression. The model included the variables age, diabetes mellitus, maximum number of bacilli, hemoglobin, total protein, serum albumin, absolute lymphocyte count, serum iron and the radiological finding of cavitation. The table only describes those variables that were found associated with the time of conversion of the sputum once the model has been adjusted. It can be observed that being between the ages of 39- 86 (older ages), the probability of conversion is 31% lower when compared with patients of 16-24 years old (RR 0.69, 95% CI, 0.52-0.90). The other two age groups did not differ from the 16-24 age groups (reference group). The low figures of serum albumin (RR 0.71, 95% CI 0.56-0.90) and absolute lymphocyte count (RR 0.64, 95% CI 0.48-0.85) were also conditions that were independently associated with a decreased probability of sputum conversion, and finally, with the exception of the number of bacilli between 1001 and 1500, in all categories of the variable maximum number of bacilli, the likelihood of conversion was lower when compared to the category of patients who had between 3 and 500 bacilli. The lower probabilities of conversion were found with the increased number of bacilli; among 1501 to 2000 (RR 0.39, 95% CI 0.23-0.66), and 2001 to 5000 (RR 0.40, 95% CI 0.28-0.58).
In the present study, the older ages, high bacillary load, low serum albumin and absolute count of lymphocytes were related to sputum conversion time in adults with infectious pulmonary TB. The first two variables (age and bacillary load) could be considered non-modifiable factors while others could be potentially modifiable with targeted interventions. Also, a significant proportion of patients after two months of treatment had positive smear sputum, which could be an evidence of treatment failure. Various factors have been associated with delayed sputum and culture conversion in pulmonary TB. The association of older age and high sputum grade with delayed conversion was described in a tertiary care facility in Pakistan (D'Souza et al., 2018) and Tanzania (Gunda, 2017). In a large cohort of smear-positive TB cases attended to in Eden Province (South Africa), those with more than 30 years old and high bacillary load had an increased probability for non-conversion (Mlotshwa et al., 2016). It is important to consider the general population dynamics in Qatar with a significative number of young people and non – Qataris, mainly young male workers migrants from Asian, Middle East and North African countries (Al-Thani et al., 2014). The double effect of smoking behavior, Diabetes mellitus and the nutritional deficiencies as risk factors for TB and delayed conversion have been described (Bhargava et al., 2013; Putri et al., 2014; Agrawal, 2017; Nakamura et al., 2014; Shariff and Safian, 2015; Guanche et al., 2016; Long and Schwartzman, 2013; Cegielski et al., 2012; Magee et al., 2014; Tachouti et al., 2011). The low frequency of active smoker, the mandatory admission for infectious patients and the compliance with the non-smoking policy in healthcare facilities could be related to our results.
Similarly, the metabolic control of diabetes mellitus in patients admitted during the intensive phase of treatment could be a factor that contributes to improved sputum conversión (Magee et al., 2014). Alkabab et al. (2017) is a retrospective cohort study of TB patients in Virginia (USA) achieved better outcomes when early interventions in diabetic patients were introduced, including patient education and therapeutic drug monitoring and dose adjustment. The effect of malnutrition on immunity and susceptibility to infectious diseases play a cardinal role in TB (Cegielski et al., 2012). In our study, in addition to body mass index, we evaluated other indicators of nutritional status. Only, the low serum albumin was identified as a factor related to the conversion. It should be considered the nutritional behavior of the population of migrant workers in Qatar, influenced by their low income and cultural factors (e.g. many patients from Indian subcontinent follow strict vegetarian diets). Further studies will be required to evaluate selected intervention to improve the nutritional status of TB patients and its impact on patient outcomes. The absolute count of lymphocytes is not primarily a nutritional factor but could be related to the immune status in patients with an infectious process and nutritional deficiencies. The low figures of lymphocytes were related to delayed conversion, which required additional studies to clarify its role in patient recovery and possible interventions to improve it. We were not able to demonstrate any significant effect of the presence of cavitations in sputum smear conversion. The radiological finding of cavitation is observed in severe cases of the disease and is a well- known factor associated with delayed conversion (Nakamura et al., 2014; Visser et al., 2012; Magee et al., 2014).
It is important to consider in the study the following issues. As per national regulations, the patients with infectious TB follow a strictly supervised treatment in in-patient facilities until sputum conversion is achieved, during which period, smoking or drinking alcoholic beverages is not allowed. Also, the frequency of multidrug-resistant Mycobacterium TB and human immunodeficiency virus infections are very low in the patients studied. The findings of the study are comparable with other studies that describe around 80% of conversion at 2 months of treatment (Hariff, 2015; D'Souza et al., 2018). D'Souza et al. (2018) in Pakistani patients describe conversion of 91.5% in new TB patients2. Other studies describe sputum conversion of 91.7% (Rural Tanzania) (Gunda, 2017), 91.9% (Ghana) (Acquah, 2015) and 91.0% (India) (Tahir, 2006). The study had some limitations as well. First, this is a single center study. Nevertheless, it was considered in this study that there are no significant differences in the population of TB patients attended to in other healthcare facilities in Qatar. Secondly, the glycemic control and the improvement in the nutritional status were not documented on regular basis during the study period, which could provide additional information about its effect in sputum conversion. In conclusion, the factors associated with delayed smear sputum conversion in TB patients attended to in a community hospital in Western Qatar were identified. Additional studies are required to evaluate the influence of nutritional status on TB diagnosis and the poor glycemic control in conversion times as well as interventions to modify these factors to improve the patient outcomes.
The authors have not declared any conflict of interests.
The author expresses his thanks to the assistance of Mr. Carlos L Crespo Palacios for reviewing this paper.
REFERENCES
|
Agrawal Y, Goyal V, Singh A, Lal S (2017). Role of Anaemia and Magnesium Levels at the Initiation of Tuberculosis Therapy with Sputum Conversion among Pulmonary Tuberculosis Patients. J. Clin. Diag. Res. 11(6):BC01-BC04.
Crossref
|
|
|
|
Alkabab Y, Keller S, Dodge D, Houpt E, Staley D, Heysell S (2017). Early interventions for diabetes related tuberculosis associate with hastened sputum microbiological clearance in Virginia, USA. BMC. Infect. Dis. 17:125.
Crossref
|
|
|
|
Al-Thani MH, Sadoun E, Al-Thani AA, Khalifa SA, Sayegh S. Badawi A (2014). Change in the structures, dynamics and disease-related mortality rates of the population of Qatari nationals: 2007–2011. J. Epidemiol. Global Health 4:277-287.
Crossref
|
|
|
|
Bhargava A, Chatterjee M, Jain Y, Chatterjee B, Kataria A, Bhargava M, Kataria R, D’Souza R, Jain R, Benedetti A, Pai M, Menzies D (2013). Nutritional status of adult patients with pulmonary tuberculosis in rural central India and its association with mortality. PLoS One 8:e77979.
Crossref
|
|
|
|
Cegielski JP, Arab L, Cornoni-Huntley J (2012). Nutritional Risk Factors for Tuberculosis Among Adults in the United States, 1971-1992. Am. J. Epidemiol. 176:409-422.
Crossref
|
|
|
|
D'Souza KA, Zaidi SMA, Jaswal M, Butt S, Khowaja S, Habib SS, Malik AA (2018). Factors associated with month 2 smear non-conversion among Category 1 tuberculosis patients in Karachi, Pakistan. J. Infect. Pub. Health pp. 11:283-285.
|
|
|
|
Guanche GH, Castaneda MM, Rodriguez Artiles MA, Gutierrez García F, Paulino Basulto MA, Pérez Alejo A, Villanueva Arias A (2016). Factors Related with Sputum Smear Conversion Time among Tuberculosis Patients. Walailak. J. Sci. Tech. 13:251-260.
|
|
|
|
Gunda DW, Nkandala I, Kavishe GA, Kilonzo SB, Kabangila R, Mpondo BC (2017). Prevalence and Risk Factors of Delayed Sputum Conversion among Patients Treated for Smear Positive PTB in Northwestern Rural Tanzania: A Retrospective Cohort Study. J. Trop. Med. Article ID 5352906, 5 p.
Crossref
|
|
|
|
Hamad Medical Corporation (HMC) (2012). Annual Health Report, 2012. Chapter 6. Vital Health. Statistic and Preventive Medicine,
|
|
|
|
Hamad Medical Corporation (HMC) (2011). Management of Tuberculosis in Qatar. 1st ed (2011).
|
|
|
|
Holtz TH, Sternberg M, Kammerer, Laserson KF, Riekstina V, Zarovska E, Skripconoka V, Wells CD, Leimane V (2006). Time to Sputum Culture Conversion in Multidrug-Resistant Tuberculosis: Predictors and Relationship to Treatment Outcome. Ann. Int. Med. 144:650-659.
Crossref
|
|
|
|
Kanda R, Nagao T, Tho NV, Ogawa E, Murakami Y, Osawa M, Saika Y, Dois K, Nakano Y (2015). Factors Affecting Time to Sputum Culture Conversion in Adults with Pulmonary Tuberculosis: A Historical Cohort Study without Censored Cases. PLoS. ONE. 10:e0142607.
Crossref
|
|
|
|
Kim J, Kwak N, Lee HY, Kim TS, Kim C, Han SK, Yim JJ (2016). Effect of drug resistance on negative conversion of sputum culture in patients with pulmonary tuberculosis. Int. J. Infect Dis. 42:64-68.
Crossref
|
|
|
|
Kurbatova EV, Gammino VM, Bayona J, Becerra MC, Danilovitz M, Falzon D, Gelmanova I, Keshavjee S, Leimane V, Mitnick CD, Quelapio MI, Riekstina V, Taylor A m Viiklepp P, Zignol M, Cegielski JP (2012). Predictors of sputum culture conversion among patients treated for multidrug-resistant tuberculosis. Int. J. Tuberc. Lung. Dis. 16:1335-1343.
Crossref
|
|
|
|
Long R, Schwartzman K (2013). Pathogenesis and transmission of tuberculosis. In: Menzies D, ed. The Canadian Tuberculosis Standards, 7th Edition. Can. Respir. J. 2(Suppl A):9A-15A.
|
|
|
|
Magee MJ, Kempker RR, Kipiani M, Tukvadze N, Howards PP, Narayan KM, Blumberg HM (2014). Diabetes Mellitus, Smoking Status, and Rate of Sputum Culture Conversion in Patients with Multidrug-Resistant Tuberculosis: A Cohort Study from the Country of Georgia. PLoS ONE 9:e94890.
Crossref
|
|
|
|
Mi F, Tan S, Liang L, Harries AD, Hinderaker SG, Lin Y, Yue W, Chen X, Liang B, Gong F, Du J (2013). Diabetes mellitus and tuberculosis: Pattern of tuberculosis, two-month smear conversion and treatment outcomes in Guangzhou, China. Trop. Med. Int. Health 18:1379-1385.
Crossref
|
|
|
|
Mlotshwa M, Abraham N, Beery M, Williams S, Smit S, Uys M, Reddy C, Medina-Marino A (2016). Risk factors for tuberculosis smear non-conversion in Eden district, Western Cape, South Africa, 2007–2013: a retrospective cohort study. BMC Infect. Dis. 16:365.
Crossref
|
|
|
|
Nakamura A, Hagiwara E, Hamai J, Taguri M, Terauchi Y (2014). Impact of underlying diabetes and presence of lung cavities on treatment outcomes in patients with pulmonary tuberculosis. Diabet. Med. 31:707-713.
Crossref
|
|
|
|
Putri F, Burhan E, Nawas A, Soepandi PZ, Sutoyo DK, Agustin H, Isbaniah F, Dowdy DW (2014). Body mass index predictive of sputum culture conversion among MDR-TB patients in Indonesia. Int. J. Tubercul. Lung. Dis. 18:564-570.
Crossref
|
|
|
|
Shariff NM, Safian N (2015). Diabetes mellitus and its influence on sputum smear positivity at the 2nd month of treatment among pulmonary tuberculosis patients in Kuala Lumpur, Malaysia: A case-control study. Int. J. Mycobact. 4:323-329.
Crossref
|
|
|
|
Tachouti N, Nejjari C, Benjelloun MC, Berraho M, Elfakir S, El Rhazi K, Slama K (2011). Association between smoking status, other factors and tuberculosis treatment failure in Morocco. Int. J. Tuberc. Lung Dis. 15:838-843.
Crossref
|
|
|
|
Unsematham S, Kateruttanakul P (2013). Factors predicting sputum smear conversion and treatment outcomes in new smear-positive pulmonary tuberculosis. J. Med. Assoc. Thai. 96:644-649.
|
|
|
|
Visser ME, Stead MC, Walzl G, Warren R, Schomaker M, Grewal HM, Swart EC, Maartens G (2012). Baseline Predictors of Sputum Culture Conversion in Pulmonary Tuberculosis: Importance of Cavities, Smoking, Time to Detection and W-Beijing Genotype. PLoS ONE. 7:e29588.
Crossref
|
|
|
|
World Health organization (WHO) (2017). Tuberculosis country profile (Qatar).
View
|