ABSTRACT
Antenatal care is more beneficial in preventing adverse pregnancy outcomes when received early and continued till delivery. World Health Organization (WHO) recommends at least four antenatal care visits for women with no complication. Conversely, survey data from Ethiopia showed that only one third are initiated early. Thus, assessing magnitude and factors affecting antenatal care (ANC) completion is required for public health intervention planning and implementations. Accordingly, this study is conducted with the aim of assessing factors affecting ANC completion among mothers attending delivery and postnatal service in Jimma town health facilities. Institution based cross-sectional study design was employed from March to April 2016 in Jimma town. Three hundred and sixty six mothers who came for delivery and postnatal service were selected using simple random sampling technique. Interviewer administered questionnaires were used to collect data. The data were entered into EPI data version 3.1 and analyzed using SPSS for Windows, version 20. Regression analyses were used to isolate independent predictor’s antenatal completion. A total of 366 participants of the study, 364 underwent all the study components giving a response rate of 99.4%. Majority of the women (77.9%) have completed ANC service as per WHO recommendation. On a multivariable logistic regression analyses, educational status [AOR= 4.59, 95% CI: 1.2, 16.6)], women’s decision making power [AOR=1.5, 95% CI: 0.03, 0.13)], knowledge about ANC [AOR= 2.45, 95% CI: 1.19, 5.03] and service satisfaction [AOR= 2.44, 95% CI: 1.03, 5.76)] were significantly associated with ANC completion. Findings of the study showed nearly a quarter of pregnant women still did not comply with the WHO recommendation. Therefore, programmes designed for promotion of ANC should be focused on educating a mother and improvement of service.
Key words: Antenatal care (ANC) completion, antenatal care, maternal health.
Pregnancy is a crucial time to promote healthy behaviors and parenting skills. Antenatal care (ANC) can play an important role in improving maternal health through counseling prevention of delivery complications, motivating pregnant information seeking and encouraging women to have safe delivery at health institution (Ahmed and Das, 1992). During ANC visits, essential services such as tetanus toxoid immunization, iron and folic acid tablets, and nutrition education are also provided. Lack of antenatal care has been identified as one of the risk factors for maternal mortality and other adverse pregnancy outcomes in developing countries (Hollander, 1997). Moreover, a link is evident between lack of antenatal care and maternal mortality, perinatal mortality, low birth weight, premature delivery, pre-eclampsia, and anemia (Ahmed and Das, 1992; Hollander, 1997).
Globally, at least 160 million women become pregnant annually. Of these, 15% develop a serious complication. Over 30 million women in the developing world suffer from serious diseases and disabilities. When a woman dies in childbirth, her infant and any other children’s survival is threatened. Every year, an additional 2 million children worldwide are maternal orphans. It is estimated that 150,000 African women die each year from causes related to pregnancy and childbearing, and that the life time risk of dying from maternal causes for African women is in the order of one in twenty five (Di Mario et al., 2005; World Health Organization (WHO), 2012).
According to demographic survey of Ethiopia (2014), a maternal mortality ratio (MMR) of Ethiopia was estimated to be 420 deaths per 100,000 live births (Ethiopia Mini Demographic and Health Survey (EMDHS), 2014). The same report stated the major causes of maternal deaths as obstructed/prolonged labor (13%), ruptured uterus (12%), severe preeclampsia/eclampsia (11%), malaria (9%) and complications from abortion (6%). All the aforementioned risks can be prevented by early initiation of ANC and having recommended minimum ANC visit. The major supply side constraints affecting maternal health are shortages of skilled midwives, weak referral system at health center levels, lack of inadequate availability of emergency obstetrics surgery equipment and under-financing of the service (Federal Democratic Republic of Ethiopia, 2010).
The world health education (WHO) recommends a minimum of four ANC visits to accomplish the essential level of ANC for every pregnant woman based on the time references of fetus development. The first visit which is expected to screen and treat anemia, syphilis, screen for risk factors and medical conditions that can be best dealt with in early pregnancy and initiate prophylaxis if requirement is recommended to be held by the end of the fourth month. The second, third and fourth visits are scheduled at 24 to 28, 32 and 36 weeks, respectively. All pregnant women should have at least four ANC assessments by or under the supervision of skilled attendant. These should, as a minimum, include all the interventions outlined in the new WHO antenatal care model and be spaced at regular intervals throughout pregnancy, commencing as early as possible in the first trimester (WHO and United Nations Children’s Fund (UNICEF), 2003).
The content of services received and the kinds of information given to women during their ANC visits are also important components of quality care. These services raise awareness of the danger signs during the pregnancy, delivery, and postnatal period, improve the health-seeking behavior of women, orient them to birth preparedness issues, and provide basic preventive and therapeutic care (Joyce et al., 2014).
One of the strategies aimed at addressing maternal mortality in developing countries is the implementation of focused ANC (FANC), which is the care a woman receives throughout her pregnancy. World Health Organization (WHO) in 2001 issued guidance on this new model of ANC for implementation in developing countries. The new FANC model reduces the number of required antenatal visits to four and provides focused services shown to improve both maternal and neonatal outcomes (EMDHS, 2014). Globally, progress has been made in terms of increasing access and use of antenatal care, although the proportion of women obtaining minimum of four visit is too low (United Nations Population Fund (UNFPA), 2011).
The country proportion of urban antenatal care service utilization in Ethiopia is 32% whereas in Oromia it is 32.7% (WHO, 2012). No specific study has been done on the magnitude and factors that affect ANC completion in Jimma town thus far. Thus, this study aimed to identify factors affecting pregnant mothers ANC completion in Jimma town and to disseminate the research result and recommendation accordingly to the concerned body.
Study design and area
Institutional based cross-sectional study design was employed in Jimma town from March to April, 2016. Jimma town is located at 346 km south west of Addis Ababa. According to the national census of 2007, the projected total population of the town is 184925, of whom 94312 are men and 90613 women. According to this population, the number of pregnant women in Jimma town is 6287. Jimma has one governmental specialized hospital, one government general hospital, and four government health centers and from private clinics giving maternal and child health service actively throughout the year in the town.
Sample size and sampling technique
Using the proportion of urban ANC four visit service utilization in Ethiopia of 32% (WHO, 2012), a margin of error of 5% and none response rate of 10%, a sample of 368 pregnant mothers were calculated. Study subjects were selected from eight health facility in Jimma town giving delivery service throughout the year for the study population; four health facilities were selected using simple random sampling. The 2015 fiscal year number of delivery reported from the clinics were used for proportional allocation to size for each health facilities.
Data collection, procedure and analysis
Data was collected using structured questionnaire adapted after reviewing similar literature. The collected data reviewed and checked for completeness, accuracy and consistency by the supervisors and investigator and correction action was taken prior to data collection to minimize errors. After that the data was double entered into EpiData v 3.1 and validated duplicated files. The statistical analyses were performed using a computer software package (SPSS for Windows, version 21.0 (SPSS, Chicago, IL, USA). The data were checked using frequencies and cross tabulations. Descriptive statistics (frequencies, percentage, mean and standard deviation) was computed to show pictures of the data. Statistical tests at 95% of Confidence Interval were made. Those variables with P-value less than 0.25 in bivariate analysis were selected by enter methods as candidate variables (clinical importance) for multivariate analysis. Model fitness for multivariate analysis (for the final model) was assessed by Hosmer and Lemeshow Test with chi-square of 3.961, degree of freedom of 8, and p value of 0.86. Multicollinearity and interaction between independent variables were checked and removed from analysis. Multivariate binary logistic regression analysis was used to identify the predictor variables. The adjusted odds ratios together with their corresponding 95% confidence intervals were determined.
Ethical consideration
Ethical clearance was obtained from ethical review committee of the College of Health Science of Jimma University. Letter of cooperation and support from the university together with the ethical approval letter was presented to Oromia Regional Health Bureau and Jimma town administration. Successively letter of support was written to selected health facilities to get permission before the start of the data collection. Moreover, all the study participants were informed verbally about the purpose and benefit of the study along with their right to refuse. Confidentiality of the study participants was assured by using questionnaire identification number and privacy during the interview.
Socio demographic characteristics
Out of the total of 366 respondent living in Jimma town who planned to participate in the study, 364 were enrolled in the study, giving a response rate of 99.4%. ANC completion was 77.9%. Majority of the respondent were in the age between15 and 24 years old (44.5%) followed by 25 to 34 age groups (42.3%), the rest were 34 years and above. The mean ages of the respondents were 25.39±5.2 years. Majority of the respondents were Oromo ethnic groups (56.8%), followed by Dawro (17.5%) and Amhara 61 (16.7%). Most of the study subjects (94.8%) were married. Concerning respondents occupation, majority of them were house wife (55.5%) followed by private employed (30.6%) and government employed (13.9%), respectively. Majority of respondents’ (44.8%) income lies in ≤1500 birr followed by 1501 to 2999 birr (30.6%). Most mothers attended (43.2%) primary school while other (38.5%) attended secondary (12.0%). However, few (6.3) of the respondent cannot read and write as shown in Table 1.

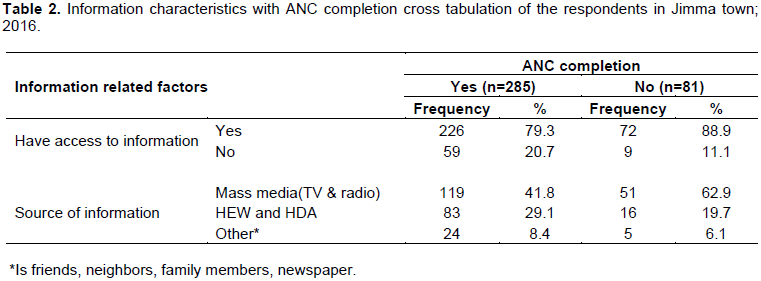
Information related factors
Regarding to information about ANC utilization; 298 (81.4%) of the respondent have access to information and from those respondent, 226 (79.3%) visited four times and above, the major source of information was mass media (both TV and Radio) 170 (46.4%), followed by HEWs and HAD 99 (27.0%) (Table 2).
Reason for not completing ANC visit
Among the total respondents included in this study, 81 (22.1%) of respondent did not completed their ANC follow-up or not visit at least four.
The major reason for not completing were due to long waiting time at health facility 23 (28.3), being expected at health 19 (23.4), not satisfied with previous visit 17 (20.9), work overload 16 (19.7), and husband disproval 6 (7.4).
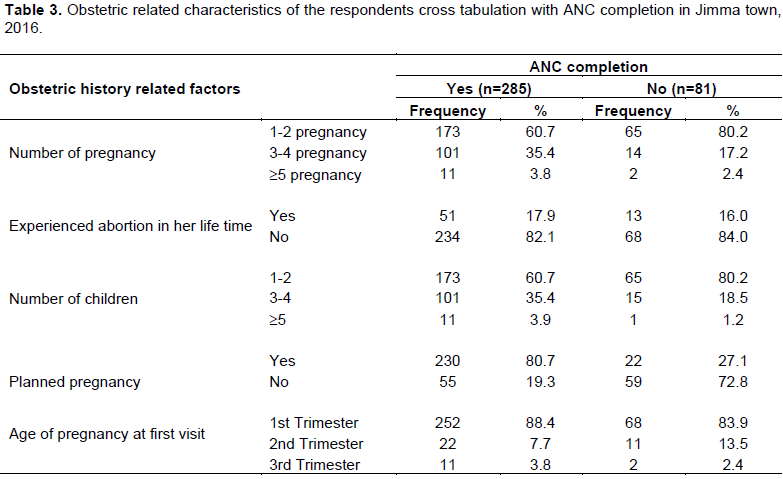
Obstetric history related factors
From the total respondents, majority of them 238 (65.0%) 1 to 2 children; followed by 115 (31.4%), 3 to 4 children. Sixty four (17.5%) of them experienced abortion in their life time; of these, 51 (79%) completed ANC visit for the recent pregnancy and 13 (20%) not completed. The proportion of respondents who made their first ANC within the recommended time (before or at 16 weeks of gestation) is 320 (87.4%). Majority of the respondents completing ANC were respondent who had 1 to 2 children; 173 (60.7%) followed by 3 to 4 children 101 (35.4%). Of those that does not complete ANC were experienced 13 (16%) of abortion in their life time. Concerning weather the resent pregnancy was planned or not, 252 (68.8%) of pregnancy was planned. Of these, 230 (80.7) completed ANC and 22 (27.1) not completed and 114 (31.1%) were not planned from these 55 (19.3) complete and 59 (72.8%) not complete ANC (Table 3).
Knowledge of respondent
The knowledge status of respondents was assessed by five knowledge related questions reviewed and adapted from different literatures. Among respondents included in this study, 140 (38.3%) women had good knowledge, whereas 226 (61.7%) of the respondents had poor knowledge.
Women’s decision making power
The decision making status of women was assessed by five decision making questions; and those women who can decide by themselves or jointly with their partners were declared as had decision making power; based on these assessment, 210 (73.6%) women who completed their ANC follow up had decision making power, whereas only 14 (17.2%) of women who did not complete ANC follow up had decision making power.
Satisfaction level of respondents
The satisfaction level of respondents was measured by nine satisfaction related questions by likert scale degree of measurement as strongly dissatisfied to strongly satisfied. Based on these, the mean score of satisfaction level was computed and become 33 ± 4.5. So, 138 (37.7%) women completing ANC service were not satisfied and 54 (14.7%) women not completing ANC were not satisfied.
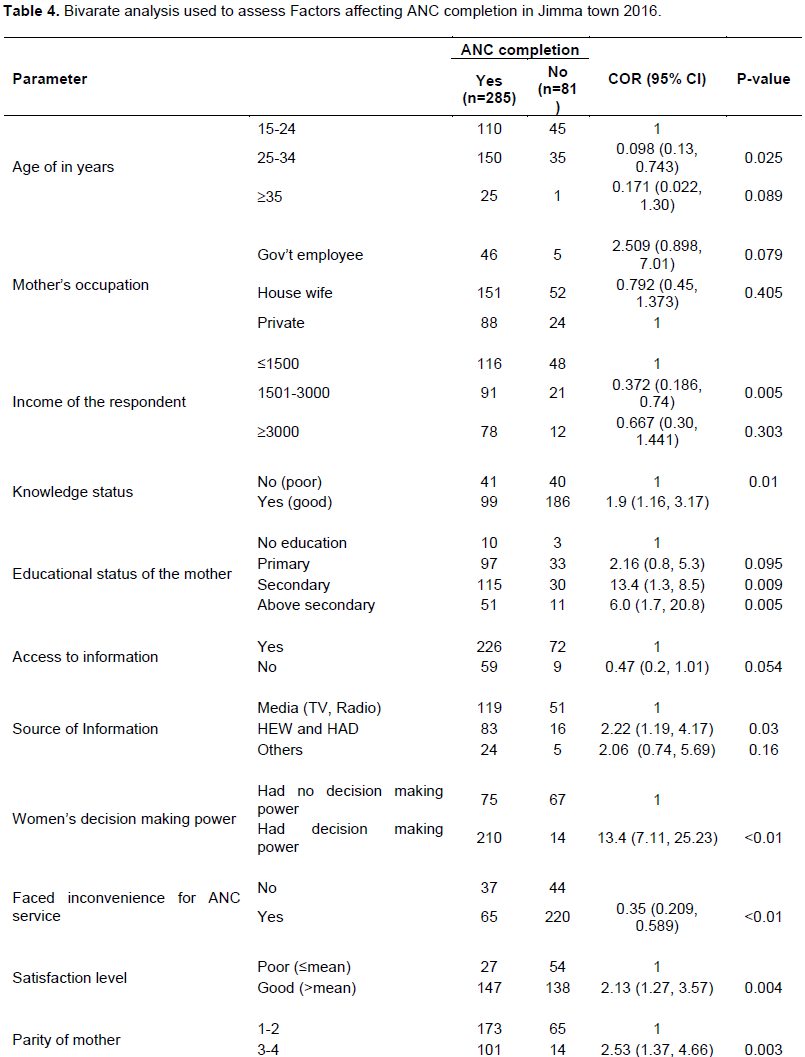
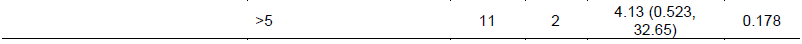
Factors affecting ANC completion
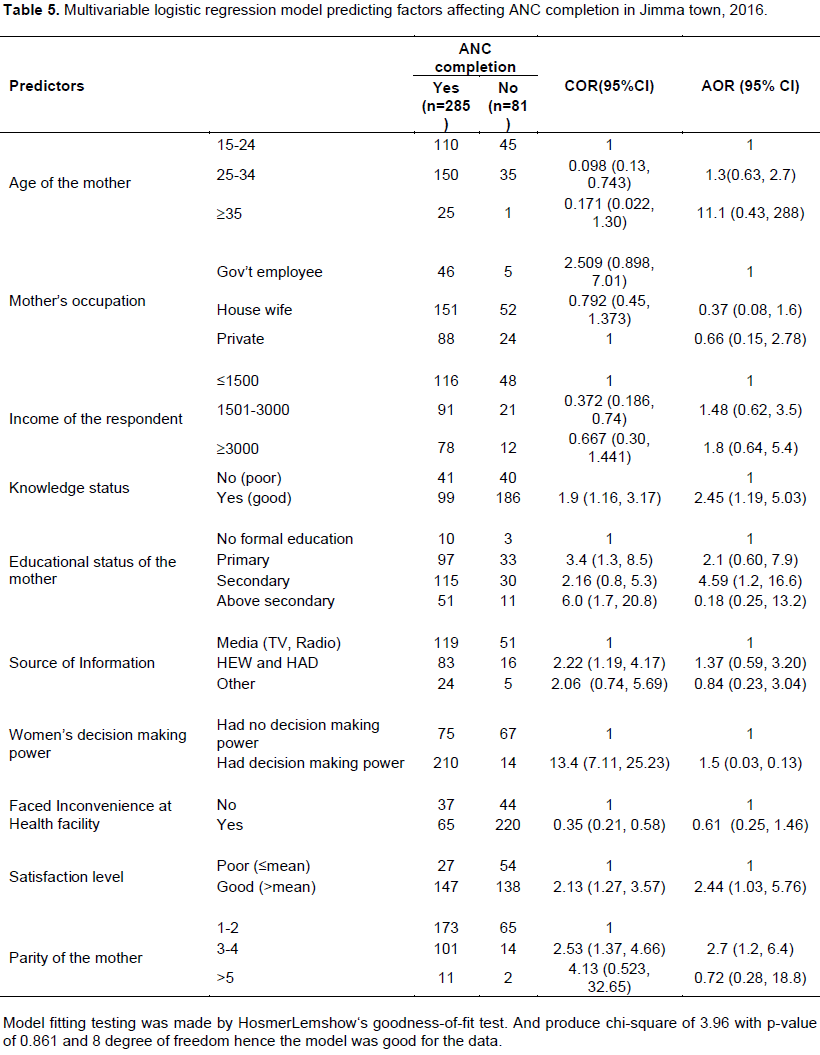
As shown in Table 4, education status of the mother, knowledge, satisfaction level and decision making power
were significantly associated with ANC completion.
On a multivariable logistic regression analyses, after adjusting for other variables, having educational status of secondary school [AOR 4.59 95% CI (1.2, 16.6)], having good knowledge about ANC completion [AOR 2.45 95%CI (1.19, 5.03)], decision making power [AOR CI 1.5 95% (0.03, 0.13)], and being satisfied with service given were 2.44 (1.03, 5.76) positively associated with ANC completion (Table 5).
This study assessed magnitude and factors affecting completion of ANC visit in Jimma town of Oromia region. According to this particular study ANC completion of women living in Jimma town were 285 (77.9%). This study finding is inconsistent with mini EDHS2014 which is 32% (WHO, 2012). The difference may be due to the time difference between current study and mini EDHS. And may be because of high coverage of health facility in the town. The finding is in line with the study done in Amhara Region Dembecha district 80% and Asossa Benshagulgumz 77.7% (Ang et al., 2010; Aregay et al., 2014). Also, consistent with the study conducted in rural West Sumatra, Indonesia which is 77.9% (Ilir et al., 2009).
The finding is significantly high comparing prospective observational study done in Zambia, 22%, Kenya, 43% and the Pakistan site (24%) (Bahilu et al., 2009).This may be due to methodological and geographical difference. The result is higher than Jimma health office report of 2015. This is may be because of the recording and reporting problem. The major reason for not completing were (32.0%) due to long waiting time at health facility (22.2%), being expected at health (19.7%), work overload, and not satisfied with previous visit. From respondents in Yem special zone, the main reasons for not utilizing ANC is that they were apparently healthy during their last pregnancy, family matters, lack of awareness, too far facility, no husband support, and long waiting time (Edward, 2011).
The proportion of respondents who made their first ANC within the recommended time (before or at 16 weeks of gestation) is 87.4%). This was significantly higher than the previous report by mini EDH 2014 which is 39.6% and Kembata Tembaro zone (31.4%) (Federal Democratic Republic of Ethiopia, 2010; Osorio et al., 2014). This may be attributed to the time difference between current study and mini EDHS survey, that there could be improvement in accessing and utilizing health care service through time and geographical variation.
Women’s decision making power is independent predictor of ANC completion; those women who had decision making power were 1.5 times more likely to complete ANC service than those who had no decision making power. Review of the literature done by USAID reported substantial restrictions on women autonomy and involvement in decision-making (Chompikul and Isaranurug, 2008; USAID, 2012). Study conducted in AbunaGndaberet also revealed that women having decision making power were 8.1 times more likely to utilize ANC than women having no decision making power and study done in Yem special woreda husband, approval is the main factor of ANC utilization (Edward, 2011; Zeine et al., 2010).
Women having good knowledge for ANC service were 2.4 times more likely to complete ANC visit than who have poor knowledge. In the study conducted in Asosa Benshagulgumz, having knowledge on ANC service was independent predictor of ANC utilization. Women who were knowledgeable on ANC service were 1.96 times more likely to utilize ANC service than women who were not knowledgeable about ANC services. Study conducted in Enderta district, Tigray, also reveals that women who had knowledge on danger signs were 2.3 times more likely to attend ANC service than those women who had no knowledge on danger signs (Ilir et al., 2009; Tekelab and Berhanu, 2014).
Maternal satisfaction on health facility services was found to be one of the predictor for ANC completion. Corroborating our finding, a study conducted in Indonesia reported pregnant women who had poor satisfaction with antenatal care services were 4.6 times more likely to inadequately utilize the antenatal care compared to those who had high satisfaction (Chompikul and Isaranurug, 2008; Aregay et al., 2014). Being satisfied on health service, delivery potentially motivates mothers to visit health facility.
Educational status of women was also found as independent predictor for ANC utilization in the study area. Having a higher educational attainment is strongly associated with high ANC completion. The results showed women who had completed secondary education were 4.5 times more likely to complete ANC follow up than those who are not educated. Many study conducted previously support this finding. A study conducted in Abuna Gndeberet also presented mothers who did not have formal education 21% times less likely to utilize ANC service than those having formal education. The finding was also consistent with study conducted in Enderta district, Tigray, who reported, women who had completed secondary school and above were 2.5 times more likely to complete ANC service than illiterate women (Aregay et al., 2014; Gurmesa, 2009). Study conducted in Yem spatial woreda also reveals that mothers who learn secondary and above were 3.9 times more likely to utilize ANC service (Amentie, 2015; Desalegn et al., 2014).
Similarly, in Nigeria, educated women are more likely to report four or more visits to ANC compared to uneducated one with odds of utilizing ANC among women who attended secondary school and above were 7.6 times more than women who were illiterate, whereas women who were able to read and write were 3.18 times more likely to utilize ANC service than women who were illiterate (Bahilu et al., 2009). Education of mother’s increases women’s enhancement knowledge regarding benefits of maternal health services. Education is likely to enhance females’ autonomy so that women develop greater confidence and capability to make decisions about their own health.
Limitation of the study
Since this study used cross-sectional study design, it does not show temporal relationship between dependent and independent variables. Due to limited literature, it was difficult for further comparison and discussion.
CONCLUSION AND RECOMMENDATIONS
This study revealed that nearly one fourth of women in Jimma town attending health facilities didnot complete their ANC service as per WHO recommendation. The major reason for not completing ANC visit were, due to long waiting time at health facility followed not satisfied with previous visit and being healthy. The proportion of mothers who made their first ANC within the recommended time (before or at 16 weeks of gestation) was very high when compared with other study (United Nations Population Fund (UNFPA), 2011; Aregay et al., 2014). Concerning factors affecting ANC completion, knowledge status, decision making power, satisfaction for health facility services and age were an independent predictors of ANC completion. For policy maker, it is better if policy makers made an effort to incorporate maternal and child health issues in school curriculum by doing that young ladies can have enough knowledge on MCH service like ANC, delivery and PNC. Making an effort towards women’s empowerment, Regional Health Bureau, Jimma town health offices continue their current and existing efforts and strengthening urban health extension workers so that mothers can have enough information about ANC completion. In capacity building for service providers by giving on job training, regular supportive supervision and taking corrective measures to ensure good governess and increasing satisfaction of the client. Health institution and service provider of health facilities have to prepare attractive and convenient maternal waiting area. Service providers should give priority for mothers to come for MCH service and by doing that decreasing waiting time and increasing satisfaction, give integrated MCH service, council and give relevant information about ANC to mothers so that the knowledge status can be increased. Urban health extension workers should create awareness to the community and refer pregnant mothers early as much as possible. For researcher, it will be more valuable if further studies will be conducted on this subject matter with alternative study design so as to find more factors associated with ANC completion.
The authors have not declared any conflict of interests.
REFERENCES
|
Ahmed FU, Das AM (1992). Three ANC visits might be the divergent point in lowering low birth weight babies in Bangladesh. 33:50-53.
|
|
|
|
Amentie M (2015). Utilization of antenatal care services and influencing factors among women of child bearing age in Assosa District, Benishangul Gumuz Regional State, West Ethiopia. Sci. J. Clin. Med. 4(3):52.
Crossref
|
|
|
|
|
Ang Y, Oshida Y, Ashid M (2010). Factors affecting the utilization of antenatal care services among women In Kham District, Xiengkhouang province, Lao Pdr. pp. 23-34.
|
|
|
|
|
Aregay A, Alemayehu M, Assefa H, Terefe W (2014). Factors associated with maternal health care services in Enderta District, Tigray, Northern Ethiopia: A cross sectional study. Am. J. Nurs. Sci. 3(6):117-125.
Crossref
|
|
|
|
|
Bahilu T, Abebe GM, Yohannes D (2009). Original Article Factors Affecting Antenatal Care Utilization in Yem Special Woreda Southwestern, Ethiopia. Ethiop. J. Health Sci. 19(1):45-50.
|
|
|
|
|
Chompikul J, Isaranurug S (2008). Factors Related to the utilization of antenatal care services among pregnant women at health centers in Aceh Besar District, Nanggroe Aceh Darussalam Province, Indonesia. J. Publ. Health Dev. 6(2):99-108.
|
|
|
|
|
Desalegn E, Mekonnen A, Abeje G (2014). Place of delivery after antenatal care: the case of Fogera. J. Gynecol. Obst. 2(1):1-6.
Crossref
|
|
|
|
|
Di Mario S, Basevi V, Gori G, Spettoli D (2005). What is the effectiveness of antenatal care? (Supplement) Copenhagen, World Health Organization (WHO) Regional Office for Europe (Health Evidence Network report, accessed 28 December 2005).
|
|
|
|
|
Edward B (2011). Factors influencing the utilisation of antenatal care content in Uganda. Austr. Med. J. pp. 516-525.
|
|
|
|
|
Ethiopia Mini Demographic and Health Survey (EMDHS) (2014). Central Statistical Agency Addis Ababa, Ethiopia. pp. 1-112.
|
|
|
|
|
Federal Democratic Republic of Ethiopia (2010). Health Sector Development Programme. 4:1-137.
|
|
|
|
|
Gurmesa T (2009). Original article antenatal care service utilization and associated factors in Metekel Zone, Northwest Ethiopia. Ethiop. J. Health Sci. 19(2):111-119.
|
|
|
|
|
Hollander D (1997). Prenatal benefits improve birth outcome among working Mexican women. Int. Family Plan. Perspect. 23(2):94-95.
Crossref
|
|
|
|
|
Ilir H, Ilirjana B, Vjosa K (2009). Antenatal Care in Kosovo Quality and access, Prishtina, Kosovo. pp. 1-53.
|
|
|
|
|
Joyce J, Moses G, Winnie K (2014). Barriers to Access and Utilization of Maternal and Infant Health Services in Migori, Kenya. Dev. Country Stud. 4(15):48-52.
|
|
|
|
|
Osorio AM, Tovar LM, Rathmann K (2014). Individual and local level factors and antenatal care use in Colombia: a multilevel Analysis. Pub. Med. 30(5):1079-1092.
Crossref
|
|
|
|
|
Tekelab T, Berhanu B (2014). Factors Associated with Late Initiation of Antenatal Care among Pregnant Women Attending Antenatal Clinic at Public Health Centers in Kembata Tembaro Zone, Southern Ethiopia . Sci. Technol. Arts Res. J. 3(1):108-115.
Crossref
|
|
|
|
|
United Nations Population Fund (UNFPA) (2011). The State of the World's Midwifery: Delivering Health, Saving Lives. pp. 1-180.
|
|
|
|
|
United States Agency for International Development (USAID) (2012). Cultural Barriers to Seeking Maternal Health Care in Ethiopia: A Review of the Literature. 2012 (December). World Health Organization. Standards for Maternal and Neonatal care: developed by the department of Making Pregnancy Safer. 2002.
View
|
|
|
|
|
World Health Organization (WHO) (2012). World health statistics. All right Reserve. 2012. P 25.
|
|
|
|
|
World Health Organization (WHO) and United Nations Children's Fund (UNICEF) (2003). Antenatal care in developing countries: Promises, achievements and missed opportunities. An analysis of trends, levels and differentials, 1990-2001. World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland.
|
|
|
|
|
Zeine A, Mirkuzie W, Shimeles O (2010). Orignal article factors influencing antenatal care service utilization in Hadiya Zone. Ethiop. J. Health Sci. 20(2):75-82.
|
|