ABSTRACT
This study aimed to determine the profile and availability of policies and guidelines as reference documents at Primary Health Care (PHC) facilities in Gaborone and its surrounding in Botswana using the World Health Organisation/Drug Action programme (WHO/DAP) Questionnaire. The Questionnaire is a standard recommended by WHO and therefore was not piloted. All 20 PHC facilities were included in the study, however, data from 18 clinics was collected and analysed. The Matron from each PHC facility was asked to name and produce as evidence, guidelines and policy documents available as reference in his/her PHC facility. Data was entered in an Excel spread sheet and percentages, averages and frequencies were used to describe the profile and availability of the documents at each facility. Fifty two different documents were available at the facilities, 50% of them were on treatment and management of diseases. The remaining 50% were distributed between general information/policy, Ante-Natal Clinic, obstetrics and gynaecological care, and family planning. Except for guidelines for treating sexually transmitted diseases (86%), availability of the other guidelines and policy documents was low (56%) or less. Policy and guideline reference information for disease immunisation and prevention were available at 4 and 13% PHC, respectively. This low availability of such important instruments may be compromising patient care in the studied PHC facilities and should be addressed. While the Ministry of Health has produced many policy documents and guidelines as reference documents for PHC providers, none of the clinics had all the documents, raising questions on what is available at the facilities as reference and guide in the prescription practices. It is recommended that ministries of health and PHC workers should ensure that necessary reference documents are available at the facilities and staff should be trained and retrained on the use of such documents.
Key words: Rational drug use, general policy documents, medical guidelines, benefits of the guidelines, health facilities.
Rational use of drugs is an essential element in achieving quality health care. The World Health Organisation (1993) has advised that “a rational use of drugs requires that patients should receive medications appropriate to their clinical needs, in doses that meet their requirements, for an adequate period of time, and at the lowest cost to them and their community”. Regardless of the availability of health practitioner and consumer-focused information, irrational use of drugs occurs in all countries causing harm by increasing morbidity and mortality rates (World Health Organisation, 1993; Lazarou et al., 1998). Many factors contribute to the high rates of adverse effects related to inappropriate drug prescriptions including errors in dispensing the drugs, monitoring adverse effects, and patient’s adherence to the regimes (Avery et al., 2002). The consequence of these is on the increase, for example leading to hospital admissions (Hurwitz, 1969; May et al., 1977; Ives et al., 1987; Grymonpre et al., 1988). With the elderly population increasing globally, this challenge is likely to be increased because of the increasing prevalence of chronic comorbidities. Therefore the need and importance of safe pharmacotherapy focusing on evidence-based medicine and quality care have become important issues on global agenda.
In an attempt to alleviate inappropriate drug use globally, the World Health Organisation has established indicators needed to systematically describe drug use in health facilities. The organisation has suggested that such indicators would allow health planners, managers and researchers to make basic comparisons between situations in different areas or at different times. The organisation has also developed drug use indicators to be used as measures of assessing the performance of a facility in three general areas of rational use of drugs in primary care: the prescribing indicators, patient care indicators and facility care indicators (WHO, 1993).
Drug therapy in primary health care is a complex field and a challenge for pharmacists, nurses, doctors, patients, and other stakeholders because it is influenced by many factors including obtaining drug information from evidence-based sources, health care worker’s experiences, and interactions with opinion makers, patients or colleagues. The need for objective drug information sources in addition to drug industry-provided information has led to the establishment of local Drug and Therapeutic Committees which on an annual basis produce and implement local treatment guidelines in order to promote rational use of drugs (Milos et al., 2014).
Facility care indicators include treatment guidelines that are important in promoting rational use of medicines because they contain decisions to be followed by health care providers. The Guidelines integrate identified health problems and respective courses of action with the clinical judgment and experience of practitioners. Globally, many guidelines have been developed over the years and have placed treatment alternatives into classes to help practitioners in decision-making on which treatment to use. In addition, treatment guidelines are aimed at standardising healthcare, raising the quality of care, reducing risk to patients, healthcare workers, medical insurers and health plans and help in achieving the best balance between cost and medical parameters such as effectiveness, specificity, and sensitivity (Grimshaw and Russell, 1993).
General practitioners (GPs) all over the world tend to operate in broad clinical areas and use various ways of collecting information from their patients using patient-oriented care questions. The specialists on the other hand rely on sources like printed and electronic journals, treatment guidelines and other literature; or through correspondence and networks with colleagues (Bennett et al., 2005). Although practitioners and other health care workers may be aware of the existence of guidelines, prescribing practices can vary significantly and the causes of the variation can be complex differing from one clinic to another and from one country to another depending on the training backgrounds (Roumie et al., 2007), attitude and perceptions of care and the existing resources.
This report is part of a study conducted to investigate drug use practices at Primary Health Care (PHC) facilities in Gaborone, Tlokweng and Mogoditshane in Botswana as an attempt to create a baseline data on prescribing practices at PHC facilities in the selected study areas. This report focuses on determining the profile and availability of important treatment guidelines and national treatment policies that guide prescribing practices in the studied PHC facilities. The main aim of this part of the study is to map the profile and identify gaps on availability so that appropriate interventions can be developed for improving health care.
This is cross-sectional descriptive study carried out between November and December, 2014 using the WHO/DAP drug use indicators guidelines (WHO, 1993). The World Health Organisation recommends that “where there are fewer than 20 facilities in a geographical or administrative region to be studied, all facilities should be included in the sample”. There are 20 PHC facilities in the selected study area (Gaborone, Tlokweng and Mogoditshane districts) and all were included in the study. For easy understanding and communication with the practitioners at the PHC facilities, the World Health Organisation Questionnaire for collecting facility indicators (WHO, 1993) was used after being translated into Setswana, the local language. The Matron from each PHC facility was asked to list and produce the treatment guidelines and policy documents available at his/her PHC facility. The information on treatment guidelines and policy documents provided was used to determine the profile of the documents. Based on broad clinical and public health practices, the documents were grouped into seven broad categories. The categories included documents/guidelines related to management and treatment of diseases, general reference information (for example, Safe Motherhood, Botswana Treatment guidelines, British National Formulary, Enrolment Criteria for the National Rehabilitation Programme, Botswana National AIDS, Drug and Related Substances and policy documents), disease prevention, family planning, immunisation, obstetrics and gynaecological conditions and ante-natal care (ANC). Data were entered in an Excel spread sheet for analysis. The percentages, averages and frequencies were used to describe and analyse the data. Validity of the results was assured by data collected by trained health sciences university students and close monitoring of the processes and data analysis by experienced researchers. Ethical clearance was sought from the University of Botswana Institutional Review Board (Ref: URB/IRB/1506) and the Ministry of Health granted the project permit (Ref: PPME.13/18/87) to carry out the study. Permission to have access to the Primary Health Care facilities was obtained from the District Health Management Team in Gaborone. All respondents were asked to consent before the interviews.
There are 20 Primary Health Care facilities in the Gaborone City Council clinics, including Gaborone, Mogoditshane and Tlokweng. A total of 18 facilities took part in the study which brought the access rate to 90%. Two PHC facilities were excluded because one was under rehabilitation therefore out of service, while the other had no patients at the time of the study and the clinic staffs were on leave. Gaborone district constituted the majority 13 (72%) of the clinics followed by 3 (16%) clinics in Mogoditshane and two (11%) clinics in Tlokweng. Data from the 18 clinics were analysed.
The profile of guidelines and policy documents available at the PHC facilities in the studied clinics
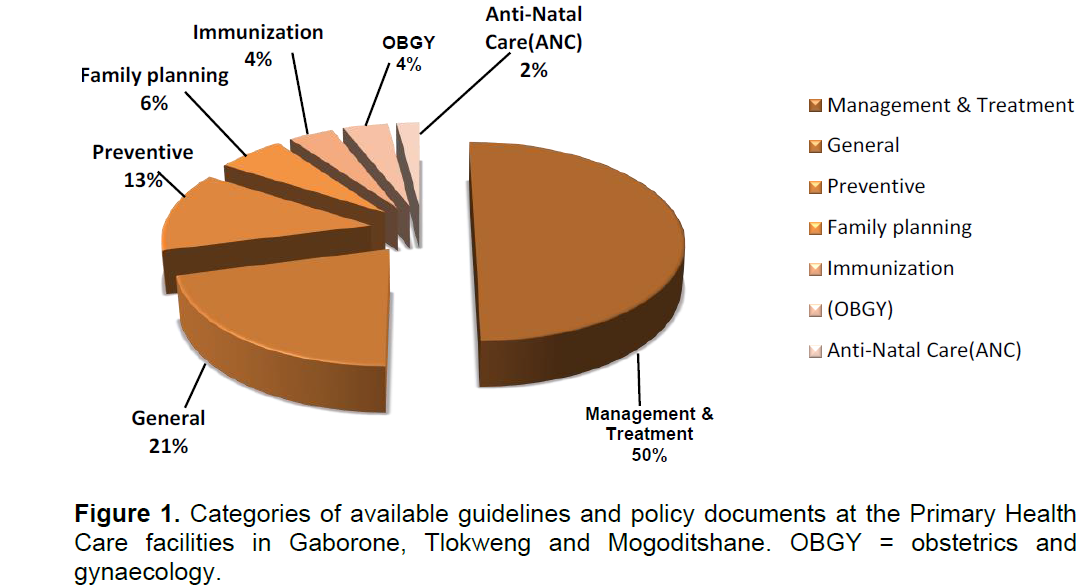
Figure 1 shows the profile of the guidelines and policy documents available at the PHC facilities. Fifty two documents were identified from the facilities and the majority (90%) were found in the offices of the Matron therefore not easily accessible in the consulting rooms. Similarly, most facilities had one copy of the documents explaining why they were kept in the Matron’s offices. The Management and Treatment category accounted for 50% of all documents available in the facilities followed by the general documents category 11 (21%). The types of the general and policy documents are shown in Table 1. The guidelines on prevention and family planning provide practitioners with definitions, general information, processes and operational procedures for early detection and prevention of diseases. Preventive and family planning documents accounted for 13 and 6%, res-reactively while immunisation and obstetrics and gynaecology each accounted for 4%. Antenatal care documents accounted for 2%.
Available general guidelines and policy documents
The general guidelines and policy documents are the basic documents prepared by the Ministry of Health and they provide the framework and guide based on local and international standard of care and practices. The distribution of the general documents category is shown in Table 1. Most expected general documents like HIV/AIDS treatment, TB treatment and the Botswana treatment guidelines were hardly available in most facilities. However, the British National Formulary was found in 50% clinics followed by the Botswana National HIV/AIDS Guidelines at 7(39%) of the clinics. The Botswana Treatment Guidelines (2007) was found in only 6(33%) facilities and the remaining, including guidelines like the Botswana Community TB Care Policy, PMTCT Programme and Baby Care Assessment were found in between 6 and 17% of the facilities.
Available guidelines on disease prevention
The highest proportion of availability of guidelines on disease prevention was that of the TB/HIV Active Case Finding Tool Guideline 4(22%) followed by Disease and Control Strategies (Measles) Guidelines, and the Pap Smear Results Management Algorithm Guidelines each found in 3(17%) facilities. Other essential guidelines were hardly available in most of the facilities as indicated in Figure 2.
Available guidelines on family planning
Figure 3 shows that out of the 18 facilities, the guideline (Botswana Family Planning Procedures for Service Providers (Rev, 2012) was available at 5(28%) clinics followed by the guide to family planning and counselling 4(22%). The Methods of Contraception (an important document for empowering women to make choices on contraception) was available at 3(17%) of the clinics.
Available guidelines on the management and treatment of diseases
Figure 4 shows the distribution of the guidelines on the management and treatment of diseases at the facilities. Except for the guidelines for the management of STIs found in 16(89%) facilities the other guidelines were available in about half of the facilities.
Available guidelines on the management of obstetrics and gynaecology, conditions
Figure 5 shows that 2(11%) facilities had the clinical classification and management of abortion, and only 2(11%) had the guidelines for the management of hypertensive disorder of pregnancy. The documents were not found at other facilities.
A medical guideline is a document used in guiding decisions and determining criteria for diagnosis, prevention, management, and treatment of diseases in specific areas of healthcare. In the history of medicine such documents have been developed and been used for thousands of years (Kane, 1995). Usually, the documents are subjected to reviews depending on emerging conditions and disease trends. Healthcare providers are therefore required to know and have access to the medical guidelines of their profession and have the right to decide whether or not to follow the recommendations of a guideline depending on the disease conditions and trends. Lack of and non-accessibility to such reference resources (guidelines) has a potential to lead to irrational prescribing including misuse of antibiotics with consequent emergence of microbial drug resistance. It is increasingly recognised that overuse of antibiotics enhances the development of antibiotic resistance, increasing morbidity and mortality as well as increasing costs (Goossens, 2006; Costelloe et al., 2010; Sabuncu et al., 2009; Kesselheim and Outterson, 2010; Barnett and Linder, 2014).
The WHO warned that the rates of resistance among nosocomial and community acquired infections are high and need to be addressed (WHO, 2014). In fact, common infections are becoming more difficult to treat with standard drugs compelling prescribers to shift to newer approaches (Fagnan, 1998; WHO, 2001; Falagas et al., 2008; WHO, 2014). The option to go on the more expensive second-line and third-line therapy increases the cost with serious consequences on the provision of healthcare especially in the developing and middle income countries (Hassali et al., 2015). It has previously been reported that inappropriate use of antibiotics may be escalated by limited adherence to guidelines among physicians in a number of countries and non-adherence to guidelines is thought to be more prevalent among physicians in the public sector (40%) than private-for-profit sector facilities at <30% (Holloway et al., 2013; MdRezal et al., 2015). A study in Malaysia’s private ambulatory care clinics (third highest category facility) showed high antibiotics utilisation compared to public primary health care centres (WHO, 2012). These findings led to the introduction of drastic measures by the Government of Malaysia and other institutions; including publication of national antibiotics guidelines, mobile phone application to facilitate and promote access of the guidelines by health care workers (Pharmaceutical Service Division, 2015).
The Ministry of Health (MOH), United Republic of Botswana is mandated with oversight and delivery of health services for Batswana. It is responsible for the formulation of policies, regulations, norms standards and guidelines of health services. The ministry is also a major provider of health services through a wide range of health facilities and management structures. MOH provides primary health care services through District Health Management Teams (DHMTs). DHMTs are responsible for the operation of a network of health facilities, hospitals, clinics, health posts and mobile stops as well as community based preventative and promotional services (www.gov.bw/en/Ministires--Authorities/Ministry of Health-MOH/A). Over the years, the government has developed several policy documents and guidelines aiming at harmonising prescribing, treatment and prevention practices at the health facilities in the country.
It was anticipated that most of the general policy documents and guidelines would be available in most of the PHC facilities in and around the capital city, Gaborone. However, it was found
in this study that there was a paucity of these documents and guidelines at the PHC facilities. This paucity of documents may be worse than reflected in this study because the fact that each clinic has at least two consulting rooms was not taken into account. The finding that the documents were in single copies produced from the Matron’s offices suggest that these resources are inadequate and not readily accessible which may lead to serious health care consequences in busy clinics where health care workers attend to many patients and have little access to reference documents.
The two major findings in this study were firstly that most (50%) of the existing general and policy documents and guidelines focused on management and treatment. Because of the emphasis on prevention rather than cure policy, it was anticipated that documents on prevention would contribute significantly to the proportion of available documents. On the contrary, prevention and immunisation documents together accounted for only 17% of the documents. This finding may be a reflection of emphasis on treatment of diseases rather than on prevention. Secondly, not all documents and guidelines are available at all primary healthcare facilities. The low availability of the guidelines at PHC facilities raises questions on why some of the key guidelines and policy documents are not available at all clinics and what practitioners use as reference resources in their practices? These questions need to be answered through a qualitative study. Such answers will provide an in-depth overview of the PHC facilities and the available resources guiding prescribing practices at that level.
The principal benefit of guidelines is to improve the quality of care to patients and communities. Ensuring availability of guidelines at all time has now become more pressing. The 2014 Ebola outbreak in West Africa has taught the global community on the need for immediate action to establish global capacity to: prevent, detect and rapidly respond to biological threats like Ebola. In 2014, countries developed eleven lines of effort in support of the Global Health Security Agenda Action packages designed to outline tangible, measurable steps required to prevent outbreaks, detect threats inreal time, and rapidly respond to infectious disease threats (http://www.cdc.gov/globalhealth/security).
These can effectively be achieved through among others, strengthening training and deployment of an effective bio-surveillance workforce. The workforce however, would require clearly written documents and guidelines to keep them up to date. The documents should be short, focused, reader-friendly and written in a language that is easily understood. In addition, health care worker at PHC facilities should be well trained and educated regarding essential guidelines and initiatives to maximise the benefits of the drugs they prescribe. The findings reported in this study suggest that the quality of care to patients may be compromised by suboptimal availability of some essential policy documents and guidelines in most of the PHC facilities in Gaborone, Tlokweng, and Mogoditshane. This shortage of policy documents and guidelines is likely to be worse in areas further away from Gaborone, the capital city. A study of the more remote PHC facilities will clarify this. It is recommended that similar studies should be done in other PHCs in the country and the ministry of health should take full responsibility on regular basis to ensure availability of important guidelines at healthcare facilities and replenish where some of the documents are torn or lost.
Since similar findings are likely to be found in other countries, these findings provide evidence-based information on some of the challenges at PHCs and the Ministries of Health should ensure regular training and retraining of healthcare providers on the use and interpretation of guidelines and policy documents; and determine links of the training with outcomes. Healthcare providers on the other hand should be encouraged to make use of the policies and guidelines; and should on regular basis take stock of the existing documents with the view to ensure that facilities are stocked with necessary policy documents and guidelines.
.
The cross-sectional nature of the study in more closely monitored health facilities may not reflect the extent of the challenge in availability and access of relevant guidelines that are required to improve the performance of the health workers at the primary health care facilities in Botswana, and generalisation to other countries. A repeated survey including some remote PHC facilities would provide some reasonable extent of availability and non-availability of the necessary tools in such facilities.
The authors have not declared any conflict of interests.
This study was funded by the University of Botswana Office for Research and Development (ORD). The authors greatly appreciate the Ministry of Health for granting the Permit to carry out the study.
REFERENCES
|
Avery AJ, Sheikh A, Hurwitz B, Smeaton L, Chen YP, Hoard R, Cantril J, Royal S (2002). Safer medicines management in primary care. Br. J. Gen. Pract. 52 Suppl:S17-22.
|
|
|
|
Barnett ML, Linder JA (2014). Antibiotic prescribing for adults with sore throat in the United States, 1996-2010.JAMA Intern. Med. 174(1):138-140.
Crossref
|
|
|
|
|
Bennett NL, Casebeer LL, Kristofco R, Collins BC (2005). Family physicians' information seeking behaviours: a survey comparison with other specialties. BMC Med. Inform Decis Mak. 22:5-9.
|
|
|
|
|
Costelloe C, Metcalfe C, Lovering A, Mant D, Hay AD (2010). Effect of antibiotic prescribing in primary care on antimicrobial resistance in individual patients: systematic review and meta-analysis. BMJ. 340:c2096.
Crossref
|
|
|
|
|
Fagnan L (1998). Acute sinusitis: a cost-effective approach to diagnosis and treatment. Am. Fam. Physician. 58(8):1795-1802.
|
|
|
|
|
Falagas ME, Grammatikos AP, Michalopoulos A (2008). Potential of old generation antibiotics to address current need for new antibiotics. Expert Rev Anti Infect Ther. 6(5):593-600.
Crossref
|
|
|
|
|
Global health security agenda: Getting ahead of the curve on epidemic threats (2014). Fact Sheet. 26th September.
|
|
|
|
|
Goossens H, Guillemot D, Ferech M, Schlemmer B, Costers M, van Breda M, Baker LJ, Cars O, Davey PG (2006). National campaigns to improve antibiotic use. Eur. J. Clin. Pharmacol. 62(5):373-379.
Crossref
|
|
|
|
|
Grimshaw JM, Russell IT (1993). Effect of clinical guidelines on medical practice: a systematic review of rigorous evaluations. Lancet 342(8883):1317-1322.
Crossref
|
|
|
|
|
Grymonpre RE, Mitenko PA, Sitar DS, Aoki FY, Montgomery PR (1988). Drus-associated hospital admissions in older medical patients. J. Am. Geriatr Soc. 36(12):1092-1098.
Crossref
|
|
|
|
|
Hassali MA, Kamil TK, MdYusof FA, Alrasheedy AA, Yusoff ZM, Saleem F, Al-Tamimi SK, Wong ZY, Aljadhey H, Godman B (2015). General practitioners' knowledge, attitude and prescribing of antibiotics for upper respiratory tract infections in Selangor, Malaysia: findings and implications. Expert Rev. Anti Infect. Ther. 13(4):511-520.
Crossref
|
|
|
|
|
Holloway KA, Ivanovska V, Wagner AK, Vialle-Valentin C, Ross-Degnan D (2013). Have we improved use of medicines in developing and transitional countries and do we know how to? Two decades of evidence. Trop. Med. Int. Health 18(6):656-664.
Crossref
|
|
|
|
|
Hurwitz N (1969). Predisposing factors in adverse reactions to drugs. Br. Med. J. 1(5643):536-539.
Crossref
|
|
|
|
|
Ives TJ, Bentz EJ, Gwyther RE (1987). Drug-related admissions to a Family Medicine In-patient Service. Arch. Intern. Med. 147(6):1117-1120.
Crossref
|
|
|
|
|
Kane RL (1995). Creating practice guidelines: the dangers of over-reliance on expert judgment. Law Med. Ethics. 23(1):62-64.
Crossref
|
|
|
|
|
Kesselheim AS, Outterson K (2010). Fighting antibiotic resistance: marrying new financial incentives to meeting public health goals. Health Aff (Millwood). 29(9):1689-1696.
Crossref
|
|
|
|
|
Lazarou J, Pomeranz BH, Corey PN (1998). Incidence of adverse drug reactions in hospitalised patients: A meta-analysis of prospective studies. JAMA. 279(15):1200-1205.
Crossref
|
|
|
|
|
May FE, Stewart RB, Cluff LE (1977). Drug interactions and multiple drug administration. Clin. Pharmacol. Ther. 22(3):322-328.
Crossref
|
|
|
|
|
MdRezal RS, Hassali MA, Alrasheedy AA, Saleem F, MdYusof FA, Godman B (2015). Physicians' knowledge, perceptions and behaviour towards antibiotic prescribing: a systematic review of the literature. Expert Rev. Anti Infect. Ther. 13(5):665-680.
Crossref
|
|
|
|
|
Milos V, Westerlund T, Midlöv P, Strandberg EL (2014). Swedish general practitioners' attitudes towards treatment guidelines - a qualitative study. BMC Fam. Pract. 15:199.
Crossref
|
|
|
|
|
Pharmaceutical Service Division. National Antibiotic Guideline (NAG), 2nd Edition (2015).
|
|
|
|
|
Roumie CL, Elasy TA, Wallston KA, Pratt S, Greevy RA, Liu X, Alvarez V, Dittus RS, Speroff T (2007). Clinical inertia: a common barrier to changing provider prescribing behaviour. JtComm J. Qual Patient Saf. 33(5):277-85.
|
|
|
|
|
Sabuncu E, David J, Bernede-Bauduin C, Pepin S, Leroy M, Boelle PY, Watier L, Guillemot D (2009). Significant reduction of antibiotic use in the community after a nationwide campaign in France, 2002-2007.PLoS Med. 6(6):e1000084. United Republic of Botswana, Ministry of Health.
Crossref
|
|
|
|
|
WHO (World Health Organisation) (1993). How to investigate drug use in health facilities: Selected drug use indicators. Geneva: WHO/DAP.93.1 Publications.
|
|
|
|
|
WHO (World Health Organisation) (2001). WHO global strategy for containment of antimicrobial resistance.
|
|
|
|
|
WHO (World Health Organisation) (2012). The evolving threat to antimicrobial resistance: options for action.
View.
|
|
|
|
|
WHO (World Health Organisation) (2014). Antimicrobial resistance: global report on surveillance.
View.
|
|