ABSTRACT
Cognitive impairment is the major health problem particularly in elderly with type 2 diabetes mellitus. The aim of this study was to determine the magnitude of cognitive impairment and associated factors among type 2 diabetics in Jimma University Specialized Hospital, 2016. Comparative cross sectional study was employed among 105 type 2 diabetes mellitus patients and 105 matched healthy individuals at Jimma University Specialized Hospital using consecutive sampling technique. Mini-mental state examination scale was used to measure cognitive function. Frequency, independent t-test, and logistic regression were carried to present data. Variables with p≤0.05 were considered as significant association between dependent and outcome variables. Prevalence of cognitive impairment among type 2 diabetes mellitus was higher than healthy individuals (53.3%). Age, occupations, fasting blood glucose level, and type of treatment options for diabetics were the predictors of cognitive impairment among type 2 diabetes mellitus patients. The prevalence of cognitive impairment among type 2 diabetes mellitus patients was significantly higher than non-diabetes study participants. This study was intended to offer information on cognitive impairment and associated factors among type 2 diabetes mellitus patients to concerned bodies in designing diagnosis and management strategies particularly focusing on counseling in preventing risk factors.
Key words: Cognitive impairment, type 2 diabetes mellitus, mini-mental state examination, Ethiopia.
Diabetes mellitus (DM) is a chronic endocrine disorder due to disturbance of insulin hormone. Type 2 diabetes mellitus (T2DM) accounts for 90 to 95% of all varieties of DM worldwide. The rise of blood glucose level beyond the physiologic limits would result in complications to different body parts including central nervous system, which is the center of cognition (American Diabetes Association, 2013).
Cognition refers to information processing and application of knowledge which encompasses focused attention, executive function, recall, processing language and making decisions (Anderson et al., 2001; Tomar, 2012). T2DM leads to disturbances of brain metabolites (Rajani et al., 2015) and neurotransmitters which are vital for cognition. Memory function appears to be affected in patients with T2DM (Van Harten et al., 2007). Two large cohort studies confirmed that being a diabetic would increase the probabilities of developing cognitive impairment by 1.3 times as compared to non-diabetic populations (Okereke et al., 2008; Tiwari et al., 2012). Predictors of cognitive impairment as evidenced from the study in Pakistan (Musleh et al., 2014) and in India (Sengupta et al., 2014) were age, sex, educational level, area of residence, marital status, unemployment, poverty and chronic illness like hypertension and DM. A study in Korea showed a higher prevalence of cognitive impairment among elderly T2DM patients and predictors were age, educational background and systolic blood pressure (Lee et al., 2014; Mavrodaris et al., 2013). An observational study in 2011 at Tikur Anbesa Referral Hospital, Ethiopia, showed 45% prevalence of cognitive impairment (29.6% mild and 15.4% moderate) among T2DM patients (Tefera et al., 2013).
The largest proportion of the population in Jimma zone which is found in the southwestern part of Ethiopia, chew a plant with its main ingredient, nicotine (neurostimulant), called khat (35.8%), smokes cigarette (11.2%) and consumes alcohol (43.4%) (Lee et al., 2014). Thus, with the aforementioned background and due to many other risk factors, it was expected that cognitive impairment among T2DM patient in the current study area would be high. In addition, the current study would fill the knowledge gap in the area; to the authors’ best knowledge, no study had been done in Jimma town that shows the association between cognitive impairment and diabetes.
Lastly, findings from this study may help local, regional and federal policy makers and health professional give attention to integrative health approach to minimize the burden of health problems associated with T2DM. So, the purpose of this study was to determine the impact of diabetes mellitus on human cognition and associated factors that increase the risk of cognitive impairment among T2DM patients in comparison to healthy controls.
Study setting, design, and population
Institution based comparative cross-sectional study design was employed at Jimma University Specialized Hospital (JUSH) diabetic clinic, Jimma town, located at 352 km Southwest of Addis Ababa, Ethiopia. Data collection was carried out from March 25 to April 25, 2016. All T2DM patients aged 30 years and above attending JUSH Diabetic clinic, having the duration of 1 year and above from diagnosis and all relatively healthy individuals who came to JUSH diabetic clinic and matched for age, sex, and educational level were included. Individuals with gross hand tremor, blindness, deafness, hyperlipidemia, traumatic brain injury and family history of dementia were excluded.
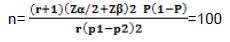
The sample size was determined using two population proportion formula with the assumption of P1 = 45% (Tefera et al., 2013) and P2=26% (Vertesi et al., 2001), and confidence level of 95% with power of 80%.
Where, n = sample size, p1 = proportion of T2DM with cognitive impairment, p2 = proportion of non-diabetes people with cognitive impairment, Zβ = standard normal variate for power, Zα = standard normal variate for level of significance, p1-p2 = effect size, P = pooled proportion, that is, average proportion (p1+p2)/2, r = ratio of number of participants of cases to controls (1 in this case). For each group, the sample size (n) was 100. After adding a non-response rate of 5%, the total sample size for each group was 105. Consecutive sampling technique was used to select both T2DM patients and healthy control individuals. During the data collection period, there was a total of 1853 DM patients registered for follow-up at JUSH diabetic clinic.
Data collection procedure
Data were collected using pretested interviewer-administered questionnaire which consisted of sociodemographic characteristics, substance use, physical measurements of height and weight, medical history and adapted standardized mini mental state examination (MMSE) for cognition assessment (Tefera et al., 2013). A MMSE evaluates orientation (10 points), registration (3 points), attention and calculation (5 points), recall (3 points), language and praxis (9 points; naming, repetition, 3-stage command, reading, writing and copying) (Vertesi et al., 2001). Diabetes-related questions were filled by reviewing the patients’ medical chart as well as testing for fasting blood sugar (FBG) format at the Medical Laboratory Department where patients often get to obtain the baseline FBG status during their routine checkup. International Diabetic Federation cut off points for body mass index (BMI) and blood pressure (BP) and the American Diabetic Association cut off points for fasting blood glucose were used to obtain the baseline BMI, BP and FBG.
Ethical consideration
Ethical clearance was obtained from the Institutional Review Board of Jimma University, College of Health Sciences and Letter of Cooperation was obtained from Jimma University and JUSH. Written informed consent was taken from the study participants to start data collection. Any identifiable issues were eliminated to ascertain confidentiality.
Statistical analysis
Data were checked for its completeness then entered to Epi data version 3.1 and exported to SPSS version 20.0 for windows. Descriptive statistics, independent t-test, and logistic regression model were done. Variables having a p ≤ 0.05 in the independent t-test were considered as statistically significant and p-value < 0.25 in the binary logistic regression was considered as a candidate for multiple logistic regression. From multiple logistic regression, exposure variables with a p-value < 0.05 with 95% confidence interval were declared as predictors for cognitive impairment.
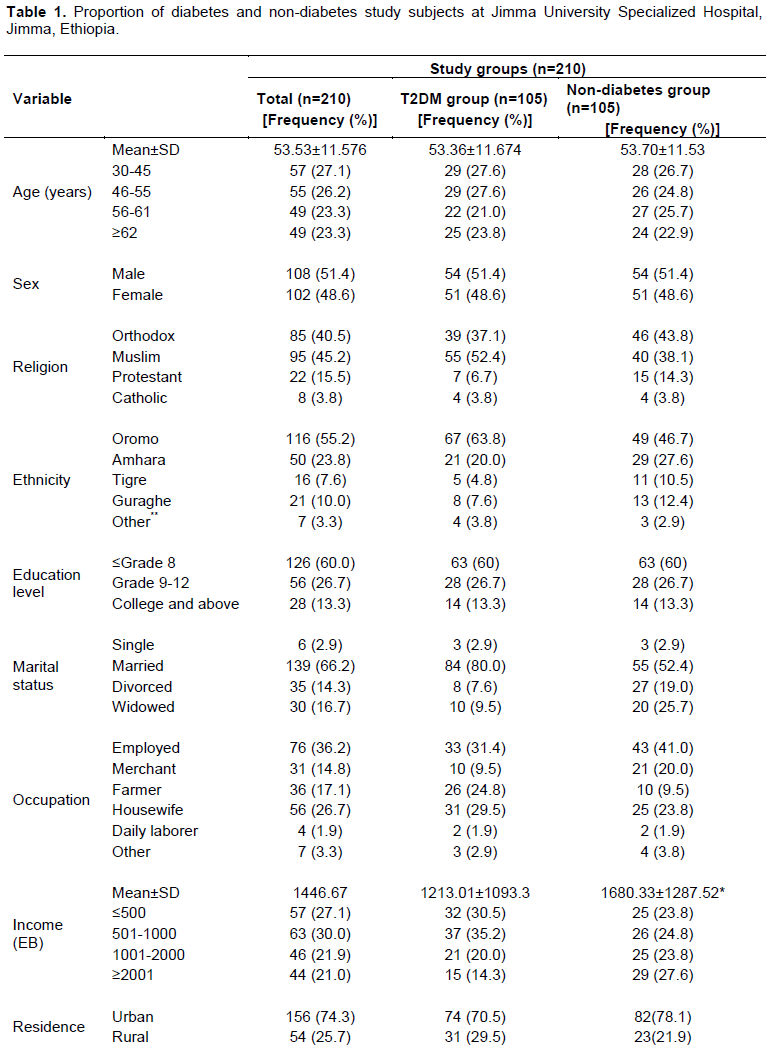
Socio-demographic and economic characteristics of the study participants
A total of 210 study participants with an equal proportion of T2DM patients and healthy controls were involved. Male to female ratio was 1.06 and majority of respondents 57 (27.1%) were in the age range of 30 to 45 years. Non-diabetes study subjects had a higher income than T2DM patients. Moreover, the mean body mass index was significantly higher among T2DM patients than non-diabetes study subjects as predict (Table 1).
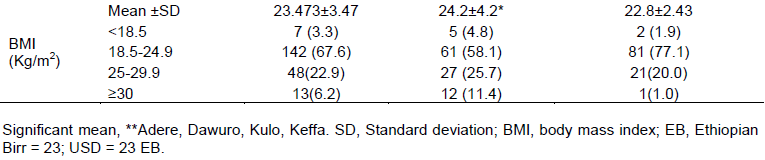
Substance use profiles of study participants
As shown in Table 2, 55 (52.4%), 33 (31.4%), and ten (9.5%) of the T2DM patients had a lifetime of khat chewing, alcohol drinking, and cigarette smoking, respectively compared to 41, 43.8 and 5.7% among healthy subjects. However, from each category, the current proportion of khat chewing, alcohol drinking, cigarette smoking was 34 (61.8), 11 (33.3%), and 2 (20%), respectively compared to 53.5, 39.1, and 33.3% among the healthy subjects (Table 2).
Cognitive impairment among T2DM patients and healthy controls
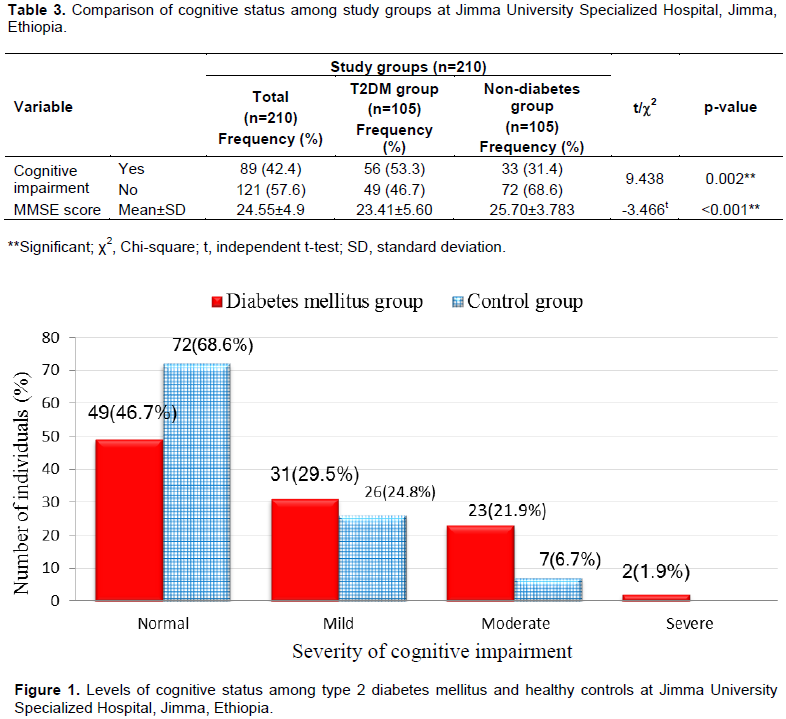
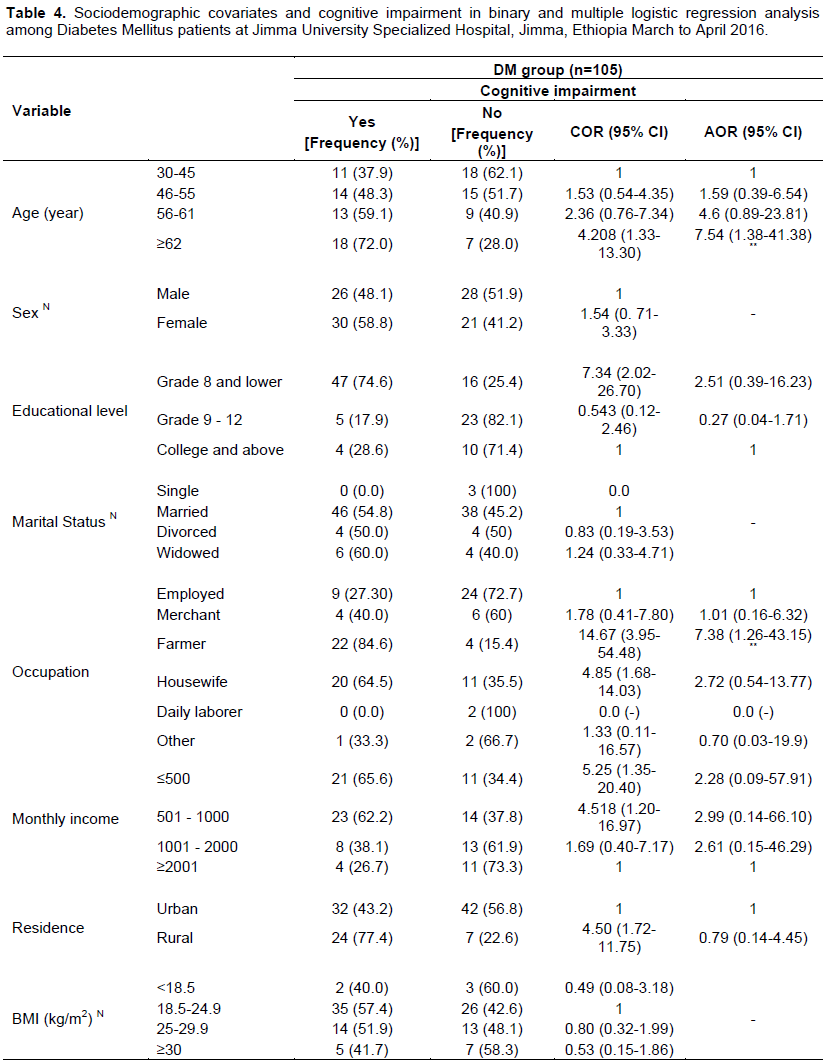
The joint education adjusted MMSE score of the study participants using the independent t-test, was 24.55 and significantly (p<0.001) lower MMSE was observed among T2DM patients compared to the non-diabetic study participants. The burden of cognitive impairment among T2DM patients was significantly higher than for non-diabetes study participants (53.3% versus 31.4%) (Table 3). Table 3 compares the severity of cognitive impairment among T2DM patients with healthy individuals; mild 31 (29.5%) versus 26 (24.8%), moderate 23 (21.9%) versus 7 (6.7%), and severe 2 (1.9%) versus 0 (0%) (Figure 1).
Clinical archives of T2DM patients
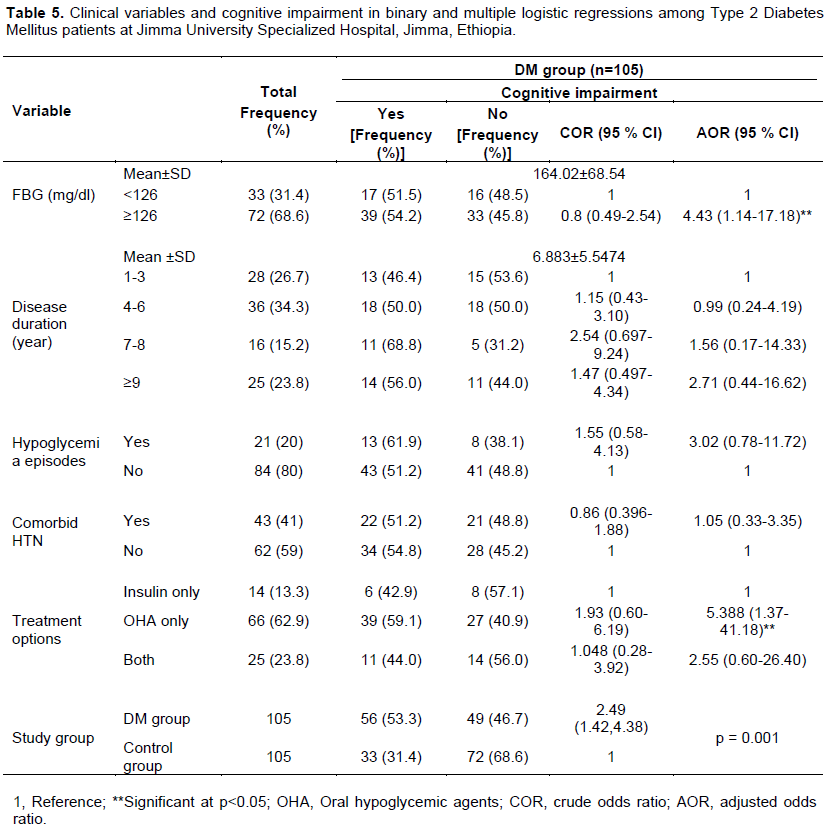
The mean duration of diabetes and FBG level were 6.9 years (SD±5.5) and 164.02 mg/dl (SD±68.54), respectively. The most (11, 68.8%) affected people were with 7 to 8 years of disease duration. Seventy-two (68.6%) had hyperglycemia (≥ 126 mg/dl) at the time of data collection; whereas 21 (20%) T2DM patients had history of hypoglycemia (<126 mg/dl) and 43 (41.0%) individuals had comorbid hypertension. Sixty-six (62.9%) T2DM patients rely on oral hypoglycemic agents, whereas 25 (23.8%) used both insulin and oral hypoglycemic agents (Table 4).
Predictors of cognitive impairment among T2DM patients
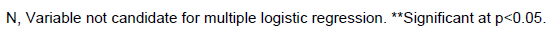
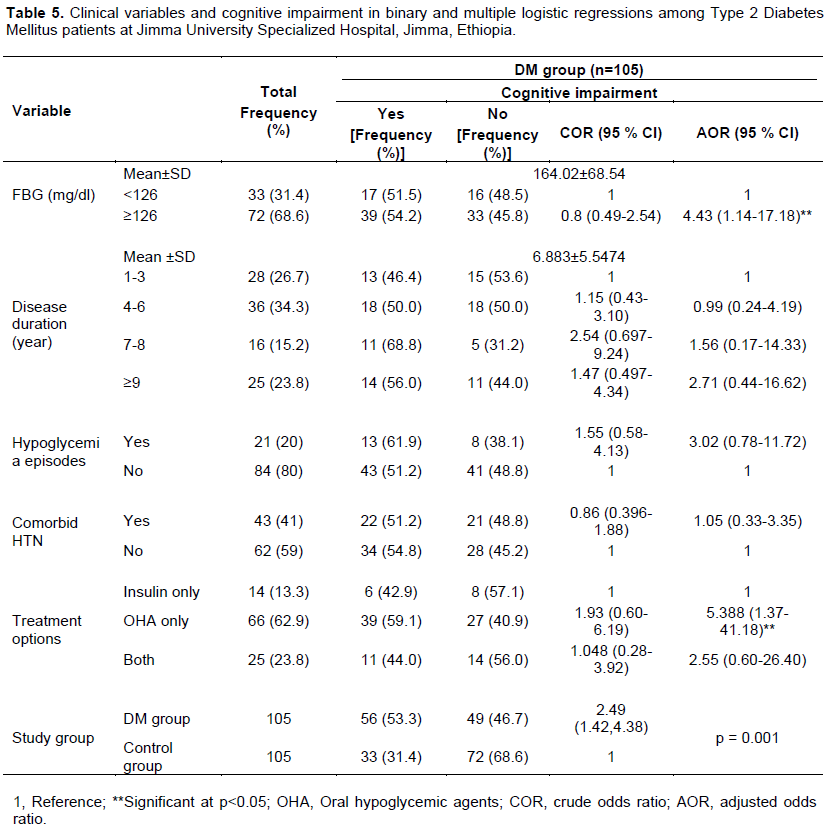
In the multiple logistic regression analysis, participants’ age and occupation, FBG level and treatment options were significantly associated with cognitive impairment. T2DM patients aged ≥62 years and being a farmer by occupation were higher odds for cognitive impairment by 7.5 times [AOR= 7.54, 95% CI (1.38, 41.38)] compared to those age ≤45 years and by 7.38 times [AOR=7.38, CI (1.26-43.15)] compared to employees T2DM patients (Table 4). Moreover, cognitive impairment among T2DM patients who had FBG level greater than or equals to 126 mg/dl is 4.4 times [AOR=4.43, 95% CI (1.14, 17.18)] as likely as cognitive impairment among T2DM patients with FBG level below 126 mg/dl. Furthermore, the odds of cognitive impairment among T2DM patients who used only oral hypoglycemic agents as a treatment option are 5.4 times [AOR=5.39, 95% CI (1.37, 41.18)] the odds of cognitive impairment among T2DM patients who used insulin (Table 5). Substance use related variables were tested for crude association with cognitive impairment in binary logistic regression. Nonetheless, there was no substance related variable with p<0.25. Hence, nothing was entered into multiple logistic regression analysis.
Interpretation of this study results has the following limitations; first, the sample size was limited and the nature of the design was cross sectional. Thus, 100% certainty could not be inferred for the associations of T2DM and cognitive function. Second, the blood glycated hemoglobin, insulin, inflammatory markers and other were not measured due to lack of fund. Thirdly, brain scan was performed to see injury in the brain that might interfere with cognation as well.
In this study, the independent predictors of cognitive impairment among T2DM patients were age, occupation, FBG, and type of treatment options. Despite the higher proportion of substance use, no substance use related variables were significantly associated with cognitive impairment among T2DM patients. This study was carried out with the intension that it will offer information on cognitive impairment and associated factors among type 2 diabetes mellitus patients to concerned bodies in designing diagnosis and management strategies particularly focusing on counseling in preventing risk factors.
The authors have not declared any conflict of interests.
REFERENCES
|
American Diabetes Association (2013). Diagnosis and Classification of Diabetes Mellitus. Diab. Care 36(Suppl. 1):67-74.
|
|
|
|
Anderson RJ, Freedland KE, Clouse R, Lustman PJ (2001). The Prevalence of Comorbid Depression. Diab. Care 24(6):1069-1078.
|
|
|
|
|
Arvanitakis Z, Wilson RS, Bienias JL, Evans DA, Bennett DA (2004). Diabetes mellitus and risk of Alzheimer disease and decline in cognitive function. Arch. Neurol. 61(5):661-666.
|
|
|
|
|
Chukwuemeka O, Basil CE, Uma A, Kenna O (2015). The Prevalence of Cognitive Impairment amongst Type 2 Diabetes Mellitus Patients at Abakaliki South-East Nigeria. J. Metab. Synd. 4(1):1-3.
|
|
|
|
|
Colzato LS, Ruiz MJ, van den Wildenberg WPM, Hommel B (2011). Khat use is associated with impaired working memory and cognitive flexibility. PLoS One 6(6):1-6.
|
|
|
|
|
Eman MA, Alshanbari M, Alswat K, Almalki D (2015). Cognitive Functions Assessment among Type 2 Diabetics with and without Diabetic Foot. Int. J. Curr. Med. Res. 4(12):398-402.
|
|
|
|
|
Hamed SA, Youssef AH, Herdan O, Abd-elaal RF, Metwaly NA, Hassan MM (2013). Cognitive function in patients with Type 2 Diabetes Mellitus: Relationship to stress hormone (Cortisol). J. Neurol. Neurosci. 4(2):1-11.
|
|
|
|
|
Hoffman R, al' Absi M (2013). Concurrent Use of Khat and Tobacco is Associated with Verbal Learning and Delayed Recall Deficits. Addiction (Abingdon, England). 108(10):1855-1862.
|
|
|
|
|
Huang CC, Chung CM, Leu HB (2014). Diabetes mellitus and the risk of Alzheimer's disease: A nationwide population-based study. PLoS One 9(1):e87095.
|
|
|
|
|
Kimani ST, Nyongesa AW (2008). Effects of single daily khat (Catha edulis) extract on spatial learning and memory in CBA mice. Behav. Brain Res. 195(1):192-197.
|
|
|
|
|
Lee YJ, Kang HM, Kim NK, Yang JY, Noh JH, Ko KS (2014). Factors Associated for Mild Cognitive Impairment in Older Korean Adults with Type 2 Diabetes Mellitus. Diab. Metab. J. 38(2):150-157.
|
|
|
|
|
Lee YJ, Kang HM, Kim NK, Yang JY, Noh JH, Ko KS (2014). Factors Associated for Mild Cognitive Impairment in Older Korean Adults with Type 2 Diabetes Mellitus. Diab. Metab. J. 38(2):150-157.
|
|
|
|
|
Leibson CL, Rocca WA, Hanson VA (1997). Risk of dementia among persons with diabetes mellitus: A population-based cohort study. Am. J. Epidemiol. 145(4):301-308.
|
|
|
|
|
Li W, Wang T, Xiao S (2016). Type 2 diabetes mellitus might be a risk factor for mild cognitive impairment progressing to Alzheimer's disease. Neuropsy. Dis. Treat. 12:2489-2495.
|
|
|
|
|
Logroscino G, Kang JH, Grodstein F (2004). Prospective study of type 2 diabetes and cognitive decline in women aged 70-81 years. BMJ 328:5480.
|
|
|
|
|
Mavrodaris A, Powell J, Thorogood M (2013). Prevalences of dementia and cognitive impairment among older people in sub-Saharan Africa: A systematic review. Bull. World Health Organ. 91(10):773-783.
|
|
|
|
|
Musleh UK, Mujeeb E, Pervez S, Lalani Z, Raza B (2014). Assessment of Cognitive Status in Type 2 Diabetes. Int. J. Collab. Res. Int. Med. Public Heal. 6(8):235-246.
|
|
|
|
|
Ojo O, Brooke J (2015). Evaluating the Association between Diabetes, Cognitive Decline and Dementia. Int. J. Environ. Res. Public Health 12(7):8281-8294.
|
|
|
|
|
Okereke OI, Kang ÃJH, Cook NR, Gaziano JM, Manson JE, Buring JE (2008). Type 2 Diabetes Mellitus and Cognitive Decline in Two Large Cohorts of Community-Dwelling Older Adults. Am. Geriatr. Soc. 56(6):1028-1036.
|
|
|
|
|
Rajani S, Reddy IY, Archana R (2015). Effect of type 2 diabetes mellitus on brain metabolites by using proton magnetic resonance spectroscopy: A systematic review. Int. J. Pharm. Biol. Sci. 5(4):1118-1123.
|
|
|
|
|
Ryan CM, Fried MI, Rood JA (2006). Improving metabolic control leads to better working memory in adults with Type 2 diabetes. Diab. Care 29:345-351.
|
|
|
|
|
Sengupta P, Benjamin AI, Singh Y, Grover A (2014). Prevalence and correlates of cognitive impairment in a north Indian elderly population. South-East Asia J. Public Heal 3:135-143.
|
|
|
|
|
Sengupta P, Benjamin AI, Singh Y, Grover A (2014). Prevalence and correlates of cognitive impairment in a north Indian elderly population. South-East Asia J. Public Heal. 3:135-143.
|
|
|
|
|
Tefera M, Muluken D, Behailu S (2013). Cognitive impairment among type 2 diabetes patients. Int. J. Med. Appl. Sci. 2(3):40-54.
|
|
|
|
|
Tiwari SC, Tripathi RK, Farooqi SA, Kumar R, Srivastava G, Kumar A (2012). Diabetes mellitus: A risk factor for cognitive impairment amongst urban older adults. Ind. Psychiatry J. 21(1):44-48.
|
|
|
|
|
Tomar S (2012). Impact of Neurobiofeedback Therapy on Cognitive Impairment Among Type-2 Diabetes Mellitus Patients. Delhi Psychiatry J. 15(2):287-293.
|
|
|
|
|
Umegaki H, Hayashi T, Nomura H, Yanagawa M, Nonogaki Z, Nakshima H (2013). Cognitive dysfunction: An emerging concept of a new diabetic complication in the elderly. Geriatr. Gerontol. Int. 13(1):28-34.
|
|
|
|
|
Van Harten B, Oosterman J, Muslimovic D, van Loon BJ, Scheltens P, Weinstein HC (2007). Cognitive impairment and MRI correlates in the elderly patients with type 2 diabetes mellitus. Age Ageing 36(2):164-170.
|
|
|
|
|
Vertesi A, Judith A, Lever D, William M, Sanderson B, Irene T (2001). Standardized Mini-Mental State Examination: Use and interpretation. Can. Fam. Phys. 47:2018-2023.
|
|
|
|
|
Wabel NT (2011). Psychopharmacological Aspects of Catha edulis (Khat) and Consequences of Long Term Use: A Review. J. Mood Disord. 1(4):187-194.
|
|
|
|
|
Wu JH, Haan MN, Liang J (2003). Impact of antidiabetic medications on physical and cognitive functioning of older Mexican Americans with diabetes mellitus: A populationâ€based cohort study. Ann. Epidemol. 13:369-376.
|
|