Full Length Research Paper
ABSTRACT
To ensure that health care is accessible to all, Community Based Health Insurance (CBHI) should be promoted and more people should be encouraged to participate in it. The aim of this study is to assess the willingness of community to enroll in community based health insurance and factors associated at household level in Siraro District, Ethiopia, 2017. Community based cross sectional study design was employed for 413 household samples. Simple random sampling method was used and face to face interviews, key informants and focus group discussions were conducted using semi-structured questionnaire. Data were entered and cleaned by EPI info and exported to SPSS. Bivariate and multivariate logistic regression was used for analysis of variables and 95% confidence level and P- value£ 0.05 was used to measure strength of association. Seventy three percent were willing to enroll in community based health insurance. Marital status (AOR=5.411, 2.448-11.959), being a member of Idir (AOR=2.618, 1.460- 4.690), being aware of community based health insurance principles (AOR=1.938, 1.083-3.464), having knowledge of inpatient services (AOR= 0.269, 0.121-0.597) and poor health status (AOR = 0.517, 0.279-0.957) were factors affecting the enrollment of community in health insurance.
Key words: Community, health insurance, willingness, enroll.
INTRODUCTION
To ensure that health care is accessible to all, Community Based Health Insurance (CBHI) should be promoted and more people should be encouraged to participate in it. A robust awareness plan should be drawn and implemented in rural areas to dispel false rumors about CBHI and enlighten the public about its merits.
Universal health coverage monitoring report in 2017 showed that many people lack essential health service and people are pushed into poverty spending too much budget. It showed that in the entire worlds, more than 7.3 illion people do not receive all the essential health service they needs. Over 800 million people spend at least 10% of their household budget to pay for health care and 100 million people are pushed to extreme poverty due to their health care expenditure (WHO, 2017).
Study showed that the level of awareness (13%) concerning CBHI was very low among the respondents. The general principles of CBHI were also poorly understood by the respondents (Adedeji et al., 2017). An enrolment in the CBHI scheme was reported to be 15.5% in non- successful community but 48.4% in a successful one. High enrolment was linked chiefly to increased awareness of the scheme, while low enrolment was linked to regressive contribution, failure to fit implementation to a specific area, insufficient community involvement, and lack of trust in the scheme and its management (Isaac, 2014).
In Ethiopia, Social Health Insurance (SHI) proclamation and other activities have been under taken with pilot CBHI in June 2011. The combination of CBHI and SHI will cover 50% population by the end of Health Sector Development Plan IV (HSDP-IV). CBHI is implemented into two stages (pilot and scale up) for covering more than 83.6% population. Only thirteen districts in four regions (Tigray, Amhara, Oromia, and SNNPRs) have been selected to implement the pilot of CBHI (FMOH, 2014). Implementation of this strategy through Primary Health Care (PHC) is guaranteed by access to health care. Therefore, service should be physically accessible, financially affordable and acceptable to patients. Ethiopia has been making effort to assure financial risk through the expansion of CBHI and SHI (FMOH, 2014).
Federal Ministry of Health (FMOH) in 2010 estimated that the four main sources of health care finance are local and internal donors (40%), central and local government (21%), out of pocket (37%) and employers and others are private insurance schemes (2%) (USAID, 2013). Risk pooling remains limited because of the small size of CBHI member population and going to scale remain a huge challenges for expansion service coverage and financial protection (Kesetebirhan et al., 2014).
Study showed that health insurance as a complimentary or alternative source as health care financing has become important in the developing world and it has been implemented as part of health reform program and strategy aimed towards providing effective and efficient health care for citizens, most especially for the poor and vulnerable (Azuogu and Eze, 2018). Ethiopian Health Insurance coverage is 1.25% which is very low but it is nearly four times of fourth round National Health Account (NHA), which is 0.32% (FMOH, 2014).
According to 2015 Ethiopia Health Insurance Agency (EHIA), out of 1252 non-members households 39% state that registration fee were not affordable for them to enroll, 17% did not have adequate knowledge and 12% prefer to see the scheme in action before becoming members. These show the affordability issue as the main determinant to become members to be enrolled in CBHI. Nearby physical accessibility of health facility is predictor of households in willingness to join decision. Regarding the agreement upon the benefit of CBHI scheme enrollment, almost all respondents (97.8%) agreed to be enrolled and most of the member is satisfied with CBHI schemes (EHIA, 2015).
Ethiopian Ministry of Health has a vision for sustainable development goal, equitable, sustainable, adaptive and efficient health services. To provide equitable service, the financial issue should be considered; CBHI is one of the strategies set as a policy to solve this problem and one of governmental concern in health care financing systems (Abebe et al., 2016). The aim of this study is to assess the willingness of community to enroll in CBHI and associated factors at household level in Siraro District. The study will be used by policy makers and for other districts implementation program.
MATERIALS AND METHODS
Study area, period and design
The study was conducted in February 15 to April 1, 2017 in Siraro District, one of the 13 districts under administration of West Arsi Zone Oromia Regional State of Ethiopia which is 322 km from Addis Ababa capital city Ethiopia to Southwest. Among 213,741 total population of the District, 106,870 are female population. The total households of the districts are 44,531. The district has 30 kebeles and 7 Health Centers. Siraro District is among the three Districts (Hasasa and Arsi Negelle Districts) which have been implementing CBHI as pilot in West Arsi Zone. All Seven Health Centers in the Siraro District were implementing CBHI scheme (Siraro district health office, 2016). Community based cross sectional study design was conducted.
Source and study population
All households in Siraro District were source population and selected households from 37 kebeles were study population. Governmental employees and those who were already members and paying regular premium were excluded.
Sample size and sampling technique
A sample size of 435 was used after calculation by EPI INFO stat using single population proportion taking P= 75% (Ololo et al., 2014) and considering 5% non-respondent rate. The stratified sampling was employed for representativeness of minority ethnic group in the district. Households in the kebele were selected by simple random sampling method using Community Health Information System house number. Two FGD with 12 members from different economic status, religion and community characters and five key informants interview were conducted for qualitative data.
Data collection method and tools
Data were collected by interview with semi structured and pre tested questionnaires. Data collectors were ten teachers and two supervisors were recruited from health center. Training was given for data collectors and supervisors on data collection process. Pretest was conducted on 5% sample in Arsi Negele District to clarify any ambiguities in the questionnaire. The questionnaire was first prepared in English and translated to Afan Oromo then back to English to check the consistency. Discussions were conducted every day between investigators, supervisors and data collectors. Data accuracy and completeness were checked every day by investigators and supervisors.
Data processing and analysis
Data were cleaned and edited after entering into EPI INFO 7 and then exported to SPSS version 21 for analysis. Descriptive statistics were computed and presented using frequencies, proportions, summary statistics, graphs and tables. Variables that have P-value < 0.25 on bivariate analyses were entered in the multivariate logistic regression model to identify independent predictors of CBHI. All tests were two-sided and P£0.05 was considered as statistically significant. The strength of association and precision were examined using adjusted odds ratio at 95% confidence interval. Thematic approach was used for qualitative data analysis.
Ethical consideration
The study was carried out after getting permission from ethical review board of Arsi University. Informed consent from institution and respondents was taken. Confidentiality was maintained by omitting name of respondents.
RESULTS
Socio demographic characteristics of respondents
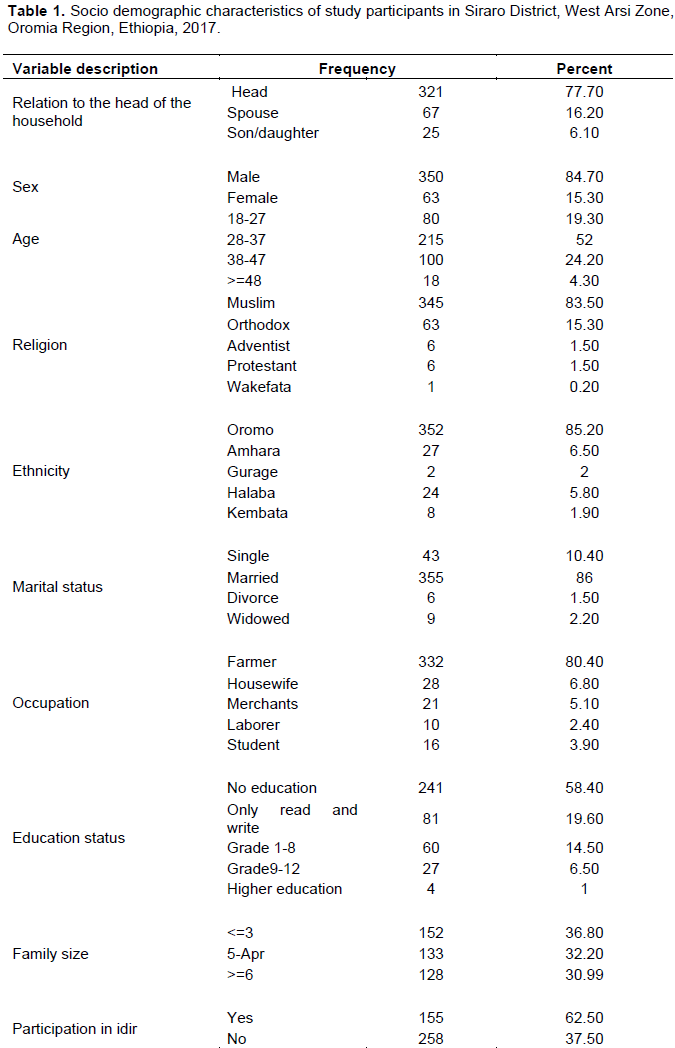
Out of 435 sample households, 413 (94.9%) participated in the study. Among them 350(84.7%) were males and 321(77.7%) were heads of household. The majority of respondents were Muslim (83.5%) and from Oromo (85.2%). With regard to marital and educational status, 355 (86%) were married and 241(58%) had no education. The mean age of the respondents was 33.62 (SD±7.3) years. The average family size was 4.48 (SD±2.27) and 258(62.5%) were idir members. With regard to occupation the majority (80.5%) was farmer and the annual median income was 5000 birr with range 400 to 40500 birr (Table 1).
Participants’ awareness and knowledge about community based health insurance
Out of 413 respondents, 405(98.1%) had information about community based health insurance from different sources. Source of information about CBHI includes Health extension workers (74%), Kebele leaders (40.4%), neighbors (18.6%), radio (9.9%), television (2.7%) and from School (1.7%). Knowledge about basic principle of CBHI includes risk sharing (56.7%), assuring equity (17.7%), solidarity (6.5%), community participation (16.9%) and not know (10.4%). The majority (91.5%) respondents had good knowledge of principles of CBHI.
Results from key informants and discussant showed that almost all community in the district heard about CBHI but knowledge about principles of CBHI were low. Community was informed about CBHI during different meeting for different purpose in the Kebele. Women Development Army (WDA) and Voluntary Community Health Workers create awareness about CBHI in addition to Health Extension Workers.
Health and health related conditions
Among 323(78%) who were ill during the last 12 month, 315 (97%) were seeking treatment and 207 (67.2%) were treated in public health center. The main reason those respondents did not seek treatment was lack of enough money (68.1%). About 17.7% medical service expense was drawing from saving account and one third (32.4%) respondents prefer health facility if the service is not expensive. For majority of respondent (79.4%) distance of public health center was less than or equal to 6o min (Table 2).
Horizontal trust and solidarity (Reciprocity)
Horizontal trust was high (34.4%), medium (6.8%) and low (23.5%) level. Furthermore, horizontal solidarity (reciprocity) was high (53.3%), medium (2.9%) and low (14.8%) level.
Willingness to enroll in community based health insurance
Of 413 participants, 304(73.6%) were willing to enroll in CBHI and 109(26.4%) were not willing to enroll. The reasons why they enroll in CBHI were access to free medical care (73.6%), security and peace of mind during illness (18.9%) and to help others (7.5%). However, the reasons why they do not enroll in CBHI were not having enough money (11.9%), preferring out of pocket payment (3.6%) and not needing CBHI (3.6%) and lack of trust in CBHI practitioner (2.2%).
According to key informants and FGD discussants, the people were willing to enroll when asked, but the actual enrollment was very low and decreasing from time to time. The main reason mentioned was the increment of the premium from 180 birr to 250 birr per household and lack of money for regular premium payment because premium payment schedule was in April and May. They do not have money to pay for registration fee and regular premium in those months since the main income of the district was agriculture. Other reason is additional 48 birr payment for son/daughter age above 18 years even if they are living with their family. The perception of key informants and discussants were: ‘God/Allah’ keeps the health of man, how would money be kept in advance before illness occurs and when I am not ill the money will not be paid back to me and why should I pay before occurrence of disease. However, others mentioned that they were happy to get treatment without thinking about financial problem when they become sick.
Factors associated with willingness to enroll in community based health insurance
Respondents who were married were 5 times more likely willing to enroll in CBHI than other groups (AOR= 5.411, CI: 2.448, 11.959). A person is a member of local insurance (Idir) is 2 times more likely to participate in CBHI (AOR = 2.618, CI: 1.460, 4.690) as well as those who know risk sharing principles of CBHI compared to those who do not know risk sharing principles of CBHI (AOR 1.938, CI: 1.083, 3.464). Respondents who mentioned inpatient was one of the service provided by CBHI are 73.1% less likely willing to enroll in CBHI than those who did not know this service (AOR 0.269, CI:0.121, 0.597). Those with poor health status were 48.3% less likely to enroll than those whose health statuses were good (AOR = 0.517, CI: 0.279, 0.957) (Table 3).
DISCUSSION
The willingness of the participants to enroll in CBHI in Siraro District was 73.6%, but the study done in Fogora District shows that 80% of the participants were willing to enroll in CBHI; study done directly on willingness to enroll in CBHI at Benchi Maji District shows that 78% were willing to enroll in CBHI scheme which were greater than this study (Adane et al., 2014; Melaku et al., 2014). This difference may be because this study did not use the CBHI schemes as it was not new to implement.
The statistical significance of marital status in this study was also supported by another study in Rwanda in 2016; CBHI evaluation study by EHIA in 2014 shows that married people were more likely to enroll in CBHI (Andinet et al., 2016; EHIA, 2015). But age, head of the household and family size were statistically significant as evidenced from Rwanda and Fogora district study mentioned above which were not significant in this study. Study done in rural China showed that reciprocity index was significantly associated and those having middle level trust were 1.47 times more likely to enroll than those with low level horizontal trust. Horizontal trust and solidarity were significantly associated with willingness in a study done at Fogora District. Study in Benchi District showed that individuals with high reciprocity were 5 times more likely to join than individuals with low reciprocity (EHIA, 2015; Adane et al., 2014; Muluken et al., 2014). This may be because the community is more exposed to CBHI. Regarding horizontal trust and solidarity not associated with CBHI this may be due to geographical variation and strong intimacy of residence.
The study about knowledge of CBHI done at household level in Iorina and Nigeria in 2014 showed that 37% of respondents were aware of CBHI and only 2.5% had good knowledge and 73% had poor knowledge about principle of CBHI. Study done in Abakalki Southeast Nigeria in 2018 showed that around 28.7% were aware of health insurance while 3.95 were aware about CBHI. In a study done in Fogora District in 2014, 64% heard about CBHI and 62.1% had good knowledge. Pilot test of CBHI evaluation survey in Ethiopia in 2014 showed that 95% were aware about CBHI which was nearly similar with that of this study (98.1%) and 91.5% had good knowledge about the principle of CBHI (Melaku et al., 2014; Adane et al., 2014; Azuogu and Eze, 2018). This high awareness may be due to health insurance was advertised and well organized under health extension worker program and political commitment in the study.
The study done in Benchi District showed that very high (12.1%) and very poor (6.2%) health status are negatively associated with willingness to enroll in CBHI. Study done in Jimma in 2009 revealed that 82% would be willing to enroll in Idir; this indicates that social boding tie was strong. Low and middle income country systematic review in 2015 showed that CBHI and out-off pocket significantly associated with enrolment and presence of chronic and acute illness episode (EHIA, 2015; Adane et al., 2014; Andinet et al., 2016; Pradeep et al., 2015). Poor health status less likely to enroll in CBHI and participation in idir was positively associated with willingness to enroll in CBHI in this study.
Satisfaction with health care service and perception of quality of health care service did not show significant difference between the two groups. The dominant reason for enrolment was to be financially secured (to access free service) and not having enough money was dominant reason for not willing to enroll in the scheme. Systematic review of factors affecting CBHI in low and middle country in 2015 showed that affordability (financial constraint and lack of money) was major constraint for scheme enrollment. Households’ satisfaction of CBHI scheme studied in Ethiopia in 2016 regarding service quality also supported this finding (Abebe et al., 2016; Pradeep et al., 2015). Service quality mentioned by key informants as reason for willingness to enroll in CBHI was supported by another study.
CONCLUSION
This study showed that almost three fourth of the households were willing to enroll in community based health insurance. Marital status, participation in Idir, risk sharing principle of CBHI, inpatient service and health status of the family were associated with CBHI enrollment. Providing quality health service through availing essential drugs, capacity building, providing training for service providers, staffing based on service load and regular evaluation of scheme activities by zonal and district health office are recommended.
CONFLICT OF INTERESTS
The authors have not declared any conflict of interests.
REFERENCES
|
Abebe S, Tushune A, Yohannes E, Tezera M (2016). Household satisfaction with a community-based health insurance scheme in Ethiopia. Bio Med Central 9(1):424. Crossref |
||||
|
Adane K, Measho G, Mezgebu Y (2014). Willingness to pay for community based health insurance among households in the rural community of Fogora District, North West Ethiopia. Science Publishing Group 2(4):6. Crossref |
||||
|
Adedeji AS, Doyin A, Kayode OG, Ayodele AA (2017). Knowledge, practice and willingness to participate in community health insurance scheme among household in Nigerian capital city. Sudan journal of Medical science 12(1):9-18 Crossref |
||||
|
Azuogu BN, Eze NC (2018). Aweness and willingness to participate in community based health insurance among Artisans in Abakaliki, Southeast Nigeria. Asian Journal of research in Medical and Pharmaceutical Sciences 4(3):2457-0754. Crossref |
||||
| Bahantunde OA, Babtunde OO, Slauadeen AG, Aderibigbe SA, Adewoye KR (2014). Knowledge of community health insurance among house hold head in rural community of Ilorne, Nigeria 3(3):800-810. | ||||
| Ethiopian Health Insurance Agency (EHIA) (2015). Evaluation of Community Based Health Insurance Pilot Schem in Ethiopia. Addis Abeba: Final Report. | ||||
| Federal Ministry of Health (FMOH) (2014). Ethiopian Health Service Utilization and Expenditure Survey briefing note. Addis Ababa, Ethiopia. | ||||
|
Isaac AO (2014). Communitry based health insurance programs and the national health insurance scheme of Nigeria: Challenge to uptake and integration. International Journal For Equit in Health 13:20 Crossref |
||||
| Kesetebirhan A, Addis T, Sentayehu T (2014). Supporting Evidence Based Descion Making: towards the acheivement of health millinium Development of Goal. In: action Papif, editor. FMOH. | ||||
|
Melaku H, Shimeles O, Berhane M (2014). Willingness to join community-based health insurance among rural households of Debub Bench District, Bench Maji Zone, Southwest Ethiopia. Bio Med Central 14:591. Crossref |
||||
| Pradeep P, Koehlmoos TP, Hossain SAS, John D, Dror DM (2015). What factors affect uptake of voluntary and community-based health insurance schemes in low-and middle-income countries? A systematic review,3ie Grantee Final Review. international initiative for impact Evaluation. London. | ||||
|
Ololo S, Megersa B (2014). Willingness to join community-based health insurance among rural households of Debub Bench District, Bench Maji Zone, Southwest Ethiopia. BioMed Central 14:591. Crossref |
||||
| Panda P, Koehlmoos TP, Hossain SAS, John D, Dror DM (2015). What factors affect uptake of voluntary and community-based health insurance schemes in low-and middle-income countries? A systematic review, 3ie Grantee Final Review. international initiative for impact Evaluation. London. | ||||
| World Health Organization (WHO) (2017). Tracking universal health caverage: 2017 global monitoring report. | ||||
| United States Agency for International Development (USAID) (2013). Ethiopia's Community-based Health Insurance: A Step on the Road to Universal Health Coverage. USAID Press Office. | ||||
| Woldemichael A, Zerfu D, Shimelis A. (2016). Community-Based Health Insurance and Out-of-Pocket Healthcare Spending in Africa: Evidence from Rwanda. | ||||
Copyright © 2024 Author(s) retain the copyright of this article.
This article is published under the terms of the Creative Commons Attribution License 4.0