ABSTRACT
The article hinged upon exploring the patterns and determinants of healthcare utilization and financing amongst particularly vulnerable tribal groups (PVTG's) in Nilgiri district of Tamil Nadu. Three PVTG’s viz Paniyas (P), Kattunayakans (KN) and Bettakurumbas (BK) are explored in the study. These groups have some quint essential features impacting the healthcare seeking behaviour e.g. Paniyas were subject to historical repression after they were brought over from Kerala as agricultural labourers culminating into their seclusion and accentuated patient provider wedge. Kattunayackans have their behaviour embedded in using magico-religious beliefs and indigenous medicines. Bettakurumbas are the other forest dwellers residing in Nilgiris biosphere reserve and contemporaneously seek institutional care. Mixed method approach (amalgamation of quantitative and qualitative) was adopted and the households were selected through two stage stratified random sampling. The health seeking behaviour was captured by running a Logit model and Blinder Oaxaca decomposition analysis was conducted to decompose the health gap amongst the tribal groups.
Key words: Health seeking behaviour, barriers to care, out of pocket expenses, vulnerable population, tribal group.
The state of health care provided around the world is an often ignored and under researched topic. A ubiquitous challenge for Indigenous communities globally is adequate access to and utilization of quality health care services. Many of these communities tend to be isolated in remote rural locations and have limited access to ambulatory, acute and specialized health care (Marrone, 2007). The variations in the availability of preventive and curative public health services amongst particularly vulnerable tribal groups are pronounced inequitable due to differences in infrastructure, human resources, supplies and spatial distribution. Burgeoning social inequality, booming private health sector, deteriorating quality of public health sector and to exacerbate, the barriers to access to healthcare has increased the differential vulnerability of tribal population. Most of the health service delivery pertaining to indigenous population has drawn flake as cultural sensitivities are not imbibed in it whereas the interpretation of illness amongst these communities is a culturally informed process. Ignoring the strong preference for cultural sensitivities jeopardizes the otherwise precarious health status of Indigenous population. In terms of health seeking behaviour; the concepts of health, healing and illness for adivasis transcends the biomedical realms and is concerned with reordering the social, environmental and spiritual balance (Eder et al., 2003). The fundamentals of health are understood from ‘functional perspective’ and as a state of dynamic equilibrium between an organism and its environment. Both patient and provider attributes have a bearing on the health seeking behaviour. Health in a tribal society is understood not as phenomena in isolation but in relation to the magico-religious fabric of existence. Also most tribal communities define health, medical care and aetiology of disease in relation to social context (Islary, 2014). Patients are more likely to adhere poorly to treatment regimens and refuse to take recommended services. Provider’s side of exchange may include bias (or prejudice) against tribals, greater clinical uncertainty when interacting with tribal patients and beliefs (or stereotypes) held by provider about the behaviour or health of tribals. Also, it is exigent to note that health seeking behaviour among tribal communities illustrates the role of social capital and reflexive communities. There is a unanimous agreement pertaining to the rudimentary health status of tribals specifically the primitive tribes owing to their isolation, geographic remoteness and more recently land alienation endangering the nutritional status and access to healthcare.
Ethnography
In Indian context the term indigenous tribe is also interchangeably used as Adavasi or ‘original inhabitants’, which literally means ‘Adi or earliest time’, and ‘vasi or resident of’. The term has further been renamed as Particularly Vulnerable Tribal Groups in India. There are 75 centrally recognized Particularly Vulnerable Tribal Groups in the country who were originally categorized as Primitive Tribal Groups. Existence of pre agricultural practices, practice of hunting and gathering, zero or negative population growth and relatively low level of literacy compared to other tribal groups are some of the quintessential features embedded in these groups. Due to changes in their ecological settings as well as outside influences, these groups are facing the problem of survival in general: either in their health and nutritional aspects or in the process of acculturation.
There are six particularly vulnerable tribal groups in Nilgiri district of Tamil Nadu of which three groups Paniya (P), Kattunayakan (KN) and Bettakurumbas (BK) are explored in the study. The Paniyas were brought over from Malabar in Kerala to the Nilgiris as agricultural labourers and are considered to be the lowest in the socio economic hierarchy whereas Kattunayakans connoting the word ‘chiefs of forests’ are considered adept sorcerers and work as healers using magico-religious herbal medicines. Bettakurumbas are the other forest dwellers residing in Nilgiris biosphere reserve that used to practice shifting agriculture before the ban was imposed on this practice. Betel leaf chewing to subdue hunger pangs is a common addiction among these tribes especially among Paniyas.
Rationale
There is pronounced difference in healthcare utilization between the tribal and non-tribal population in India in general and Tamil Nadu in particular cutting across various dimensions of healthcare. For example for maternal health dimension the utilization rates for tribal population pertaining to indicators like full ante natal check-up and institutional delivery is 41.2 and 64.7% respectively vis a vis 52.1 and 94.6% for non-tribal population (Xaxa, 2014). Majority of Scheduled Tribe population depends on the public health system, as private providers do not have any interest to work in tribal dominated areas. Reports revealed that more than three-fourths of Scheduled Tribe population seeks treatment from Government funded health facilities, as compared to only 47% of non-scheduled tribes. One-fifth of scheduled tribes seeks health care services from private sources (Xaxa, 2014). However, reports and studies have not delved particularly into indigenous tribes, rendering it imperative to conduct specific surveys to elicit the information specifically on this vulnerable group
Despite significant disparities in the health outcomes, data and research on indigenous health is often unavailable because governments and organizations have been impassive in disaggregating statistics due to lack of resources or even official policy. There’s dearth of figures to support the hypothesis of low utilization rates amongst the indigenous population. Research on tribal health so far has predominantly focused on the prevalence of morbidity, illness profile and health provision coverage rather than people’s practices, knowledge, opinions of and attitude towards health provision in tribal areas (Jain et al., 2015; Yadav et al., 2010; Kerketta et al., 2009; Santhosam et al., 2013). This paper intends to compliment the previous literature and provide further insight into factors impacting health seeking behaviour in terms of utilization and barriers to utilization with the aim to influence policy formulation, decision making and targeted service provision planning for tribal population. Another improvisation is to add a dynamic perspective in analysing individual’s health seeking behaviour and check the exposition if agents are biased towards one type of healthcare and does not switch caregivers even if treatment was ineffective for them. Another pertinent issue grappling this economically and otherwise deprived community is payments related to health; incidence and intensity of which subjects them to further impoverishment and vulnerability given the narrow band of coping mechanisms at their disposal. Financial dimension (expenditure and coping) should be explored in depth to guide the policy makers to direct the intervention towards the component where it impacts the most.
Objectives
There are two main objectives of this paper. The primary objective is to study the pattern and determinants/impediments of utilization of healthcare services amongst these tribals; and the secondary objective is to determine the factors affecting out of pocket expenditure. Also, the differences in the healthcare utilization among three tribal groups are analyzed.
Study population and location
For the present research, we have selected Gudalur block of Nilgiris district (Tamil Nadu). This is situated at the tri-junction of three states of Tamil Nadu, Karnataka and Kerala and is divided into two taluks namely Gudalur and Pandalur. According to 2011 census, population of Gudalur is 49,535 out of which 12,433 are from the Particularly Vulnerable Tribal Groups. There are six particularly vulnerable tribal groups in Nilgiris of which three groups Paniya (P), Kattunayakan (KN) and Bettakurumbas (BK) are explored in the study. These two taluks consist of 14.3 and 32% of tribal population of Nilgiris respectively and abode to 336 tribal settlements.
Sampling design and data collection
We adopted a mixed method sampling design via concurrent triangulation approach. The main purpose of this design is to offset the weakness inherent within one method with the strengths of the other method (Creswell and Plano Clark, 2007; Tashakkori and Teddlie, 2003). In this study, quantitative data was collected through survey method and the qualitative information through focussed group discussion; these two datasets were later corroborated in the interpretation and analysis section. Consistent with the objectives, the quantitative data was given more importance and qualitative data was used to complement the inferences.
For the quantitative analysis, a sample of 150 households were chosen through two stage stratified random sampling technique; whereas, qualitative information was ascertained through 12 Focused Group Discussions using a purposive sampling method. Participants who fulfilled the following eligibility criteria were included in the discussions. Firstly, the respondent should be a part of tribal group (KN, BK or P); secondly, he/she should not be less than 15 years old and thirdly, the participant should be willing to participate.
Focus groups comprised of head of Adivasi Munnetra Sangam (tribal group leader), members of tribal community, traditional healers and district officers, discussions were generally conducted in their cultural centres or educational institutions. Data was gathered through structured interview process, involving face to face conversation.
Data collection
Quantitative information was elicited by administering a questionnaire which encapsulated the information on the prevalence of disease, utilization trends and patterns, details of the inpatient and outpatient like the type of provider visited, expenditure incurred (direct and indirect) to avail the treatment and coping mechanisms to cover the expenses. While conducting qualitative analysis, user’s perspective was kept on the fore. Questions assessing the mechanism to deal with infectious and other diseases, knowledge on traditional medicine, common practices adopted by the tribal communities, community financing in case of emergency, tribal population’s adherence to modern medicine were discussed in detail.
Sampling techniques
Three sampling techniques were adopted to measure the aforementioned objectives: Descriptive statistics, logistic regression and blinder Oaxaca decomposition analysis. Descriptive statistics provided a brief summary of the entire sample population categorised into predisposing, enabling and need based indicators. Logistic regression model was used to estimate the effect of covariates on probability of utilization of healthcare services. The covariates were selected through Andersen’s framework of health care utilization (Andersen, 1968). This framework assumes that health care utilisation is influenced by predisposing factors, enabling factors and need based factors (Andersen, 1995). Decomposition analysis was conducted to measure the tribe wise differences in utilization of health care services, this was deconstructed using a “three fold” decomposition technique in which outcome difference (R) is divided into endowment effect (E), coefficient effect (C) and interaction effect (I) for logistic regression model (Jann, 2008).
R=E+C+I
In this model the contribution of group differences in predictors to the overall outcome difference was formulated from viewpoint of Group B as against Group A. The E component measures the expected change in Group B’s mean outcome if Group B had Group A’s predictor levels for the second component (coefficient effect), the differences in coefficients are weighted by Group B’s predictor levels. That is, the second component measures the expected change in Group B’s mean outcome, if Group B had Group A’s coefficients. The interaction term captures the interaction between differences in coefficients and differences in endowments. It is imperative to incorporate the interaction term because the differential between the two groups might arise due to the past exclusion culminated by historic repression or by contemporaneous one outside of health sector.
Descriptive statistics
Table 1 presents the descriptive statistics of the participant’s characteristics. The mean age of participants surveyed was 26.95 years. The percentage of male and female participants is 51.96 and 48.06% respectively. About 41% of the participants were unmarried and 47.29% of them were married. As far as the need based factors are concerned it is found that nearly 36.06% of the participants were ailing from some kind of illness of which 62% of the participants have been availing some form of health care services which includes both inpatient and outpatient services. Outpatient services were utilized by 63.7% and inpatient services were consumed by 37.3% of the participants respectively.
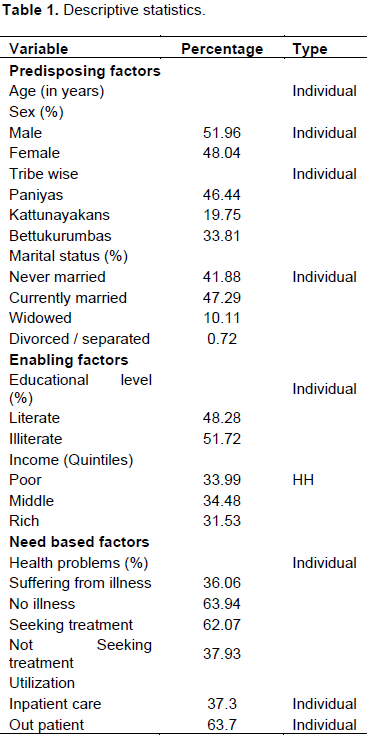
Figure 1 illustrates the reasons for non-utilization of healthcare facilities by the study group. One of the ubiquitous issues plaguing the utilization patterns are the cultural barriers with 28% of households citing it as paramount reason for not seeking care. Residing in geographically isolated places is another governing factor acting as a barrier to access and utilization as 18.2% respondents reported travelling long distances from their settlements to the point of care. Yet another important determinant of non-utilization is practice amongst the tribals to seek the treatment only in the case of emergency and severe cases. They tend to neglect the symptoms of illness as 14.55% of those who are ill do not consider it as necessary to seek care immediately after the onset of disease. Since indigenous communities are living on the brinks of marginalization thus, financial constraints inhibit the take up of health service as healthcare is a luxury good for them. According to 11% of those surveyed, inability to pay for direct and indirect costs associated with treatment is major impediment to receive the care. However, among the quality indicators only long waiting hours is the significant factor of non-utilization.
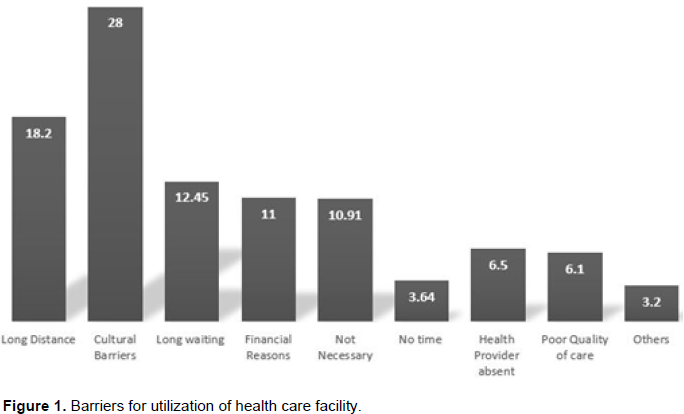
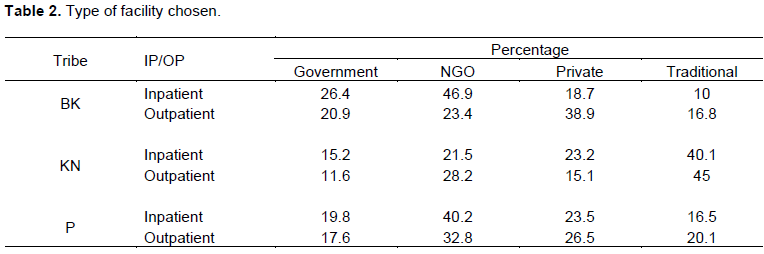
Table 2 reflects the tribe wise analysis of the type of facility chosen in case of illness disaggregated into inpatient and outpatient. It is ascertained that 46.9% of Bettukurumbas and 40.2% of the Paniya prefer hospitals run by NGO’s for hospitalisation, whereas 40.5% of kattunayakans, sought care from traditional healers. For the outpatient care, 26.4% of the Bettukurumba’s preferred Government hospitals, 45% of the Kattunayakans resorted to traditional healing and 30.8% of Paniya tribes sought care from health facilities run by NGO’s.
The utilization of public health facilities as presented in Figure 2 is subjacent as compared to both private providers and NGO’s. The participants were probed about the reasons for not seeking care in the government facility. The cardinal reason for Paniyas is reflected upon the access parameter as 32% of the respondent’s stated non -availability of required services as a reason for underutilization, 30% of the Bettukurumbas did not seek care due to long waiting hours. However, Kattunayackans feel that distance is the major impediment in seeking public health care.
Logistic regression results
The results for logistic regression are represented in Table 3 which illustrates the marginal effects of determinants of healthcare utilization on the probability of seeking care. Healthcare utilization is being explained by a consortium of independent variables ranging from predisposing, enabling and need based factors.
Effects of predisposing characteristics
Significant relation was found between household size and healthcare seeking. The probability of healthcare utilization decreases by 12.7% with the addition of one more members in the household. Similarly, the coefficient for marital status is highly significant and the marginal effects tantamount to 44.8% point decrease in the probability of utilization for a married person when compared to unmarried person. Further, it is discerned from the model that transition from being literate to illiterate leads to increase in the probability of utilization by 37.9%.
Effects of enabling characteristics
There are two enabling factors incorporated in the model, that is, income grouped into low, middle and highest income and time taken to reach the nearest health facility. Both the factors momentously explain the behavior. Participants falling in middle and highest income group expound increased probability to seek care with probability increasing to 33.7 and 55.1% for middle and highest income respectively as compared to low income group. Time taken to reach the nearest facility is also significantly found to be incongruous to visiting the facility.
Effects of need based characteristics
Among the gamut of need based characteristics reflected in the model, follow up on the warnings of health, confidence in staff and awareness in the progression of disease significantly explains the utilization behavior. Those tribals who proactively follow up on the onset of disease are 31.5% more likely to seek care when compared with tribals reporting nonchalant attitude towards the warnings. Similarly, those who are aware of diagnosis and progression of disease are 32.6% more likely to solicit care.
Blinder Oaxaca decomposition
Blinder Oaxaca decomposition as illustrated in Table 4 is used to decompose the health gap amongst the tribes. The results of the endowment effect indicate that should BK embody the same endowments as the other groups (KN and P), the health gap would increase by around 47%. The second component, the ‘coefficient’ effect measures the discrimination, if there were no discrimination and all the tribal groups were rewarded in the same way, the health gap of P would decrease by 9.3%. The interaction component captures the covariation of disparities in endowments and coefficients. The interaction effect is 4.9% and also works in the opposite direction, that is, interaction of differences in endowments and coefficients narrows the gap between the BK and P which would otherwise occur due to the endowment effect alone.
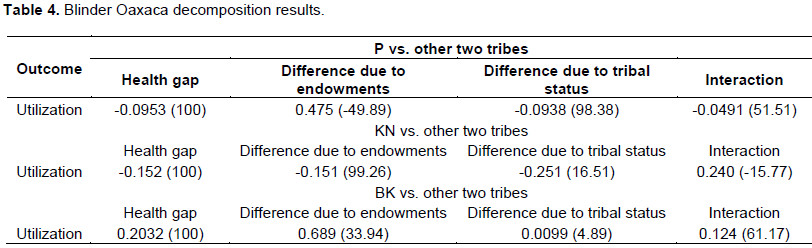
Decomposition analysis of KN with other groups reveals that should KN embody the same endowments as other groups (BK and P), the health utilization gap would decrease by around 15%. Similarly, the coefficient reveals that if there were no discrimination, and both groups were rewarded in the same way, the health gap would decrease by 25%. The interaction effect however, was found out to be 24%, that is, interaction of differences in endowments and coefficients increases the gap between the Kattunayackans and other groups which would otherwise occur due to the endowment effect alone.
Table 5 exhibits mean expenditure of Inpatient and Outpatient across various categories. The total mean per visit expenditure for the outpatient services are INR 837. It was observed that most of the contribution of outpatient expenditure was in terms of travel (INR 410) and medicines (INR 198.96). The total mean expenditure per hospitalisation visit was found to be INR 6801.87. For the inpatient services, significant contribution of expenditure was in the form of transportation (INR 2819.23) and lodging and food expenses (INR 1636.18).
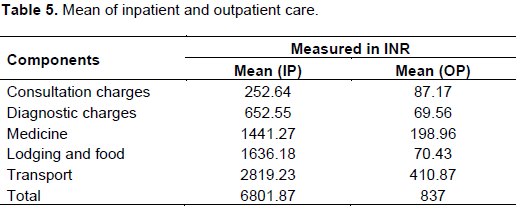
Figure 3 shows the different payment- coping strategies adopted by the households to finance the health care services availed One of the common sources of finance existing among the three tribal communities was borrowing, as 48.2% of the inpatient services were financed through borrowing and 47.2% of the households borrowed to finance their outpatient costs. Due to the very nature and magnitude of the outpatient costs, a huge chunk of it is covered through the household’s respective savings which certainly does not hold true for inpatient care expenses. 25.6% of the respondent’s managed their inpatient cost through contribution from friends and relatives, this is mainly because of the community health insurance which enables a tribe to entail financial aid in case of an emergence of a health care financial crisis, the main motto of this scheme was to ease the financial burden among the tribal population due to the exorbitant inpatient costs.
The major impediment to utilization,that is,cultural barriers are related to specific codes of etiquette/ ways of doing things and also to a much larger social structures and experiences (Braun et al., 2011). The perceptions of health and disease are multifaceted in the culturally diverse patient’s worldview and play a predominant role in augmenting cooperation and compliance to the advice given by healthcare professionals. Patients reported not fully comprehending to the western biomedical mode of treatment and ascribing higher value to their belief and indigenous systems of treatment. As narrated by the community leader of Kattunayackan tribe “In event of the illness, the decision pertaining to seek institutional care is taken by conglomeration of community members headed by the traditional healer. “Dices are rolled and combinations of numbers on the top decide the odds of whether to visit a health professional or to allow for self-healing.” Also, narratives of fear and mistrust triggered by multitude of factors such as patient- provider rift, negative past experiences, language barriers and perceived racism driving the non-utilization were reported which explains the relative relevance of culture in determining the trajectory of utilization.
The barrier of geographical isolation is exacerbated due to the presence of the reserve forest area in the region and the way in which the core and buffer regions in the reserve area is carved. The movement of people is restricted due to the fact that entire reserve areas such as in Mudhumulai is declared as the core area but the villages having an abode in such areas are not acknowledged as core, thus rendering it difficult for people to utilize the health facilities. Concomitant with this is the issue of transportation as the infrastructure and provision for same is absent in most of the areas, thereby; leading to the access of health providers quite exigent. The results are symptomatic with other qualitative study conducted on Paniya tribe in Kerala. Despite relatively good access to public healthcare, the Paniyas of Waynad have low utilization rates. Difficulties in geographical access arise due to the remoteness of their colonies, a common problem encountered by indigenous populations (Mohindra et al., 2009).
Preference for health services provided by non-governmental organizations in the area could be attributed to the free quality care and recruitment of staff from their tribes by the healthcare facilities run by them. Also, ratcheting up the uptake is the fact that these institutions are having more cultural and lingual congruence towards the tribal population thereby; leading to effective communication between the patient and provider. Lingual barriers present a formidable obstacle to accessing adequate healthcare. However, even if the provider and the patient both speak the same language, cultural values and experiences of the patient influences how they communicate their symptoms and how they perceive feedback about their health status from the provider (Marrone, 2007). Traditional healing is often the first contact of treatment among the participants as the culture of these tribes is embedded in the ethnomedicine and sorcery practices; though it varies among the tribal groups. Groups like Kattunayackans and Paniyas exhibit more preference towards the traditional healing as it is governed by the cultural practices and degree of geographic remoteness. Percentage of Kattunayackas admitted at the centres run by healers exceeds that of Bettakurumbas by four times. Upon discourse with a traditional healer, he remarked “A week ago, a girl suffering from severe diarrhea and admitted to a public hospital escaped the hospital premises as she was traumatized and deranged by modern facilities, equipment’s and environment. I treated her with herbs which restored her mental and physical state. Similarly, there is colossal variation for the outpatients as well. Even private providers are visited more frequently as compared to public health facilities. The findings are converging to the study conducted on the hill tribe population of Bangladesh where it was found that regardless of their distance and the costs that Christian missionary hospitals charged for their services; the tribal people who had access to the hospitals appreciated the quality of services, cleanliness and polite behavior of the health staff working there (Rahman et al., 2012)
The evidence is clear that social determinants of health entrenched in proximal, intermediate and distal factors influence health seeking behavior in complex and dynamic ways. Proximal factors like behavior regarding incessant substance abuse especially alcohol and tobacco consumption, delay in seeking care after the onset of disease and preferences emanating from individual psychology of fear of modern medicine and profound faith in traditional medicine is attributed to the utilization behavior. The field experience of the study is replete with incidents to establish the same. During the course of visiting the remote village in core reserve area, a snake bite case was encountered where the treatment for the patient was sought from a traditional healer despite the same physical access to the nearby public health centre. Even after the patient failed to recuperate from the placebo treatment given to him, formal institutional care was not sought, eventually leading to the death of the patient. The strong preference for traditional healing is also evident in the study conducted amongst the tribals of South Bastar in Chhattisgarh (Mahant, 2015) where 75.3% of the villager’s first preference was to seek care from traditional healer for the treatment. However, intermediate factors like community practices and cultural environment passed on to generations particularly with regards to some specific illnesses like mental health, skin disease etc. coupled with access to the healthcare significantly influences the demand for same. Our encounter with a teenage girl incarcerated by intellectual disability resounds the finding as the girl’s family perceived the experience with local public hospital as disappointing after investing time and resources and complained that the condition has deteriorated rather than improved. At the time of the visit, the family with a whiff of optimism was scrambling resources to seek care from an unskilled informal care provider located some 250 km away from their settlement therefore exhibiting that the behavior is more of guided by cultural acceptability and poor quality of institutional care in the locality. There is an encouraging evidence in terms of seeking care at hospitals run by NGO’s which is also articulated in an ethnographic qualitative study done in same region documenting people seeking treatment in non-profit private facilities for major problems (Sathyamurthi, 2016).
The study indicates that healthcare seeking behaviour of tribals is remarkably different from the non tribals. Cultural factors followed by the long distance to cover owing to the geographical remoteness and dwelling in the reserve forest areas explain most of the reasons for non-utilization. Government facilities have not found acceptance amongst these communities vis a vis private providers and traditional healers due to non-availability of services, accessibility and long waiting hours in these units. Moreover, there is resounding unanimous opinion regarding the trust wedge between the patient and providers in government run facilities. Indirect medical expenses are more as compared to the direct medical expenses as a component of out of pocket expenditure and most of the payments is financed by the borrowing from friends/relatives. Similarly, based on the logit model results consortium of factors like time taken to reach facility, household size, educational status, awareness of progression of disease and symptoms significantly explains the utilization. An integrated and holistic approach involving all stakeholders in tandem is imperative to address the complexities involving the tribal health issues. A range of culture’s negative effect on utilization can be ameliorated through addressing structural determinants of health inequities thereby, improving community awareness regarding cultural differences and augmenting cultural tolerance among health workers.
The findings are subject to certain limitations. The findings though can be generalizable to the hill tribes may not account for non-hill tribes due to geographical variations. Also, the selected sample size may not be a good representative of entire indigenous population in the state of Tamil Nadu and is suitable for local context only. Also, the distal factors like macrosocial, inequities in service delivery and organization of services were not explored in detail in the study context.
The authors have not declared any conflict of interests.
REFERENCES
|
Andersen RM (1995). Revisiting the behavioral model and access to medical care: does it matter? J. Health Soc. Behav. 36(1):1-10.
Crossref
|
|
|
|
Braun V, Clarke V (2013). Successful qualitative research: A practical guide fobeginners. Sage.
|
|
|
|
Eder K, Pú MM (2003). Model of Indigenous Maya Medicine in Guatemala. Guatemala City, Guatemala: Asociación de Servicios Comunitarios de Salud.
|
|
|
|
Islary J (2014). Health and Health seeking behavior among tribal communities in India: A Socio cultural perspective. J. Tribal Intellect. Collective India 2(1):1-16.
|
|
|
|
Jann B (2008). A Stata implementation of the Blinder-Oaxaca decomposition. Stata J. 8(4):453-479.
|
|
|
|
Jain Y, Kataria R, Patil S, Kadam S, Kataria A, Jain R, Ravindra K, Shinde S (2015). Burden and pattern of illness among the tribal communities in central India : A report from a community health programme. Indian J. Med. Res. 141(5):663.
|
|
|
|
Kerketta AS Bulliyya G, Babu BV, Mohapatra SS, Nayak RN (2009). Health status of the elderly population among four primitive tribes of Orissa, India: A clinico-epidemiological study. Zeitschrift für Gerontologie und Geriatrie. 42(1):53-59.
Crossref
|
|
|
|
Mahant SD (2015). Indigenous Traditional Healing Care: Belief and Practices among Tribals of South Bastar in Chhattisgarh: IOSR J. Humanities Soc. Sci. 20(1):49-54.
|
|
|
|
Marrone S (2007). Understanding barriers to health care: a review of disparities in health care services among indigenous populations. Int. J. Circumpolar Health 66(3):188-198.
Crossref
|
|
|
|
Mohindra KS, Narayana D, Haddad S (2010). "My story is like a goat tied to a hook." Views from a marginalised tribal group in Kerala (India) on the consequences of falling ill: a participatory poverty and health assessment. J. Epidemiol. Commun. Health 64(6):488-494.
Crossref
|
|
|
|
Rahman SA Kielmann T, McPake B, Normand C (2012). Healthcare-seeking behaviour among the tribal people of Bangladesh: can the current health system really meet their needs? J. Health Population Nutr. 30(3):353-365.
Crossref
|
|
|
|
Santhosam MA, Umesh S (2013).A Study on the Health Status of Elderly Irular Tribal Women in Kancheepuram District. IOSR J. Humanities Soc. Sci. 7(2):1-4.
Crossref
|
|
|
|
Sathyamurthi DK (2016). A Qualitative Study on the Health and Education of Primitive Tribal Groups (PTGS) of Gudalur, Tamil Nadu. Int. J. Info. Res. Rev. 3(4):2161-2168.
|
|
|
|
Yadav Rao VG, Bhat J, Gopi PG, Selvakumar N, Wares DF (2010). Prevalence of pulmonary tuberculosis amongst the baigas a primitive tribe of Madhya Pradesh, Central India. Indian J. Tuberc. 57:114-116.
|
|
|
|
Xaxa V (2014). Report on the high level committee on socio-economic, health and educational status of tribal communities of India.
|