ABSTRACT
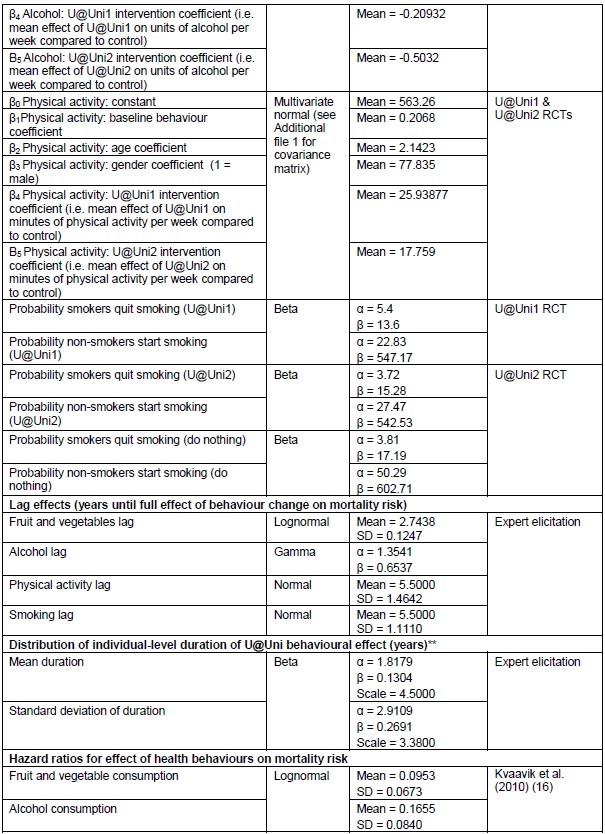
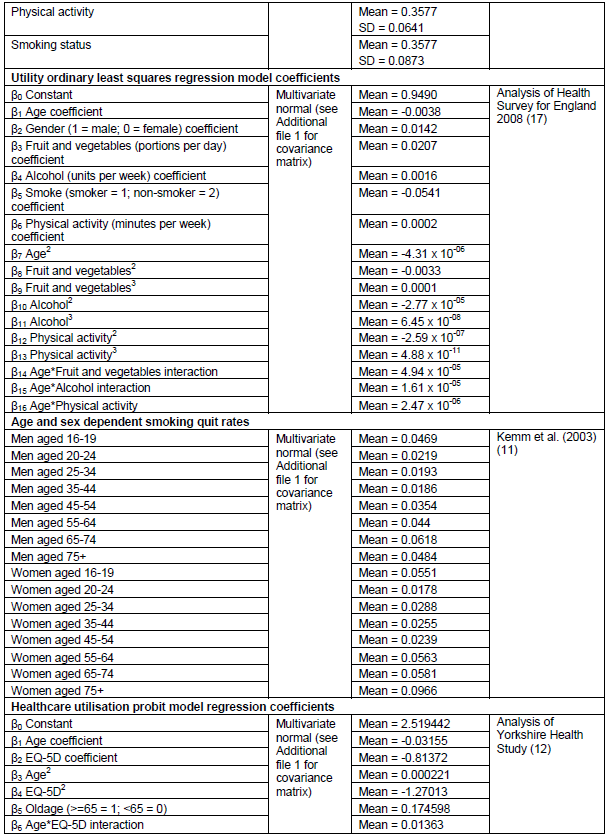
The transition to university marks a point where young people may be open to changing health behaviours such as smoking, exercise, diet and alcohol intake. This study aimed to estimate the cost-effectiveness of an updated online health behaviour intervention for new university students in the UK – “U@Uni2”, compared with both a control (measurement only) scenario and with the original intervention (“U@Uni1”). The economic analysis, based on a randomized controlled trial, comprised a detailed costing analysis, a within-trial cost-effectiveness analysis and long-term economic modelling. Cost-effectiveness of the U@Uni2 trial was estimated using 6-month data on costs and health-related quality of life. An individual patient simulation model was adapted for long-term economic analysis of U@Uni2. Probabilistic sensitivity analysis and value of information analysis accounted for uncertainty in model inputs and identified key parameters. The U@Uni2 intervention costs £45.97 per person for full implementation, £10.43 per person for roll-out in a different institution and £3.03 per person for roll-out over five years. The U@Uni2 trial was not cost-effective because marginally fewer quality-adjusted life years (QALYs) were obtained in the intervention arm than the control. However, modelled over a lifetime, U@Uni2 is estimated to produce more QALYs than control but fewer than U@Uni1, primarily due to the effect of the interventions on smoking. Roll-out of U@Uni2 is highly likely to be more cost-effective than doing nothing (ICER = £536 per QALY, 86% probability cost-effective). Decision uncertainty occurs primarily around the effectiveness of the U@Uni2 intervention and is worth up to £3.24 m. The U@Uni2 intervention is highly likely to be cost-effective to roll-out when compared with doing nothing. The results suggest that preventing uptake of smoking is the key driver of QALY gain and should be the primary target of such interventions.
Key words: Alcohol, diet, exercise, smoking, health behavior, cost-effectiveness, economic evaluation, students, university.
The National Health Service (NHS) spends billions of pounds per year treating the burden of disease caused by unhealthy lifestyle choices such as smoking, excessive drinking, lack of exercise and poor diet (The King's Fund, 2014). Many of these behaviours are adopted early in adulthood, and ultimately result in an increased risk of disease and mortality, and a reduction in health-related quality-of-life. The transition between school and university is a point when individuals are likely to change existing health behaviours and establish new habits (Friedman et al., 2008; Plotnikoff et al., 2015). U@Uni is an online intervention based upon the psychological theories of self-affirmation, planned behaviour and implementation intentions (Ajzen, 2005; Gollwitzer and Sheeran, 2006; Harris and Epton, 2009), which targets four health behaviours: smoking, drinking alcohol, eating fruit and vegetables, and physical activity in new university students. A 2012 randomized clinical trial (RCT) of a first variant U@Uni1 and a full economic analysis of U@Uni1 versus ‘measurement only’ control concluded that although the effect of the intervention on health behaviours was small, rolling out the intervention to other universities would be cost-effective (Epton et al., 2014; Kruger et al., 2014).
The U@Uni1 trial suffered from low levels of recruitment and technological problems, resulting in poor engagement with the intervention. An updated version of the intervention (U@Uni2) was designed using the LifeGuide intervention software developed by Southampton University (Yang et al., 2009), which helped to minimize technical problems. The pre-intervention baseline questionnaire was also shortened. The U@Uni2 intervention was compared with the control in an RCT of 2,623 undergraduates beginning their studies in 2013 at the University of Sheffield, United Kingdom. Results from the trial are available elsewhere (Cameron et al., 2015).
This economic evaluation aims to estimate the short-term (6-month) and long-term (lifetime) cost-effectiveness of U@Uni2, when compared with both the ‘measurement only’ control condition and also with the U@Uni1 intervention. The perspective of the study is that of the UK Department of Health.
The economic evaluation took the same format as U@Uni1 (Kruger et al., 2014), with three components: a costing analysis; a within-trial analysis; and an economic modelling analysis to estimate long-term cost-effectiveness of the U@Uni2 intervention, when compared with either the control condition or with the U@Uni1 intervention. The methods are summarized here; detailed methods are available in the online supplementary appendix.
Costing analysis
The costs of U@Uni2 were estimated using a modified version of theU@Uni1 staff costs questionnaire (Kruger et al., 2014 and Additional file 1). Staff from the Department of Psychology were asked to estimate the number of hours they had spent developing, updating and implementing the U@Uni2 intervention in addition to any non-staff costs incurred. The full economic cost of all staff time including overheads, national insurance and pension costs was estimated using the University of Sheffield’s University Research Management System. Costs were calculated at 2013 values. Three different scenarios were costed for long-term modelling. The cost of full implementation of a U@Uni2 style intervention including development costs, the cost for roll-out of the existing U@Uni2 intervention to another university, and the cost of rolling out the intervention assuming it could be used for five years with minimal updating (five-year costs). Roll-out costs were estimated in a similar manner by including the cost of developing local elements from U@Uni1 in addition to a subset of costs from U@Uni2. Five-year costs were based upon roll-out costs but were divided into an annuitized set-up cost and an annual maintenance cost. The long-term economic modelling allows three-way comparison of control, U@Uni1 and U@Uni2 interventions. To allow direct comparison, all costs from U@Uni1 were inflated to 2013 values using the consumer price index from the Office of National Statistics (ONS) (Office for National Statistics, 2014).
Within-trial cost-effectiveness analysis (short-term 6-month time horizon)
A within-trial analysis was performed by balancing the gain in QALYs accrued during the trial against the cost of healthcare and the costs of full implementation of the U@Uni2 intervention. Healthcare costs were calculated from questionnaire data that asked about healthcare utilisation during the trial period (Cameron et al., 2015). NHS Reference Costs 2012-13 (Department of Health, 2013) and the Unit Costs of Health and Social Care 2013 (Personal Social Service Research Unit, 2013) were used to assign unit costs to each healthcare source used. Data on health-related quality of life was collected at baseline, one month and six month time-points, and weighted using preference based EQ-5D values (Dolan et al., 1995). Missing data for costs and health-related quality of life was imputed using multiple imputation by chained equations (White et al., 2011). Baseline characteristics of the individuals who took part in the trial are presented in Appendix Table 1. Ordinary least squares (OLS) regression models were generated to estimate total costs and QALYs using personal characteristics as covariates.
Long-term economic modelling (lifetime time horizon)
Long-term cost-effectiveness of the U@Uni2 intervention was assessed using an adaptation of the U@Uni1 economic model (Kruger et al., 2014). The model is a population based individual patient-level simulation that models individuals selected from baseline data collected in the U@Uni2 trial. Their age, gender, portions of fruit/vegetables consumed daily, units of alcohol consumed weekly, minutes of physical activity undertaken weekly and smoking status influence their probability of dying and their estimated utility during each year of their life. The same individuals were simulated in control conditions and with the U@Uni1 and U@Uni2 interventions. Life years, QALYs and costs were discounted annually at 1.5% as recommended by NICE for public health economic evaluations (National Institute for Health and Clinical Excellence, 2012). Incremental analysis was carried out to compare each of the interventions with the control condition and with each other.
Uncertainty
Probabilistic sensitivity analysis (PSA) was carried out to estimate the probability of the interventions being cost-effective at different willingness to pay thresholds. 30,000 model runs were performed, each simulating 1000 random individuals. Expected value of perfect information (EVPI) and partial expected value of perfect information (EVPPI) were carried out, using the Sheffield Accelerated Value of Information (SAVI) online tool (Strong et al., 2014), to determine the value of further research into parameter estimation.
A series of structural sensitivity analyses were carried out to test certain model assumptions. The sensitivity of the results of the duration of intervention effect was tested by fixing the mean at values of 1, 2, 5 and 10 years. The model was also tested for the sensitivity of results to the structural updates to the model. Finally, the contribution of each of the four individual behaviors to costs and QALYs was assessed.
Costing analysis results
Costs for full implementation of the U@Uni2 intervention were estimated at £61,828 (£50,544 to £73,158, 95% confidence interval [CI]), of which £47,179 was due to previous spending on U@Uni1 and £14,649 was specific to U@Uni2. Staff cost was £27,444 in total, whilst non-staff costs comprised £34,384. This is considerably cheaper than the cost estimated for full implementation of U@Uni1 (Kruger et al., 2014), which when inflated to 2013 values came to £213,921. The reason for the large difference is due predominantly to the use of the LifeGuide software for U@Uni2 (Yang et al., 2009), which eliminated the need for costly development of a website from scratch. Given that there were 1,345 individuals in the intervention arm of the RCT, this works out as £45.97 per person (£37.58 to £54.39, 95% CI).
Roll-out costs for U@Uni2 were estimated at £15,701 (£13,555 to £17,864, 95% CI), of which £9,792 was due to previous spending on U@Uni1 and £5,909 was specific to U@Uni2. The comparable inflated costs for U@Uni1 were £30,768. The U@Uni1 costs were larger due to website maintenance that the U@Uni1 site required. The mean number of UCAS acceptances per UK institution in 2013 was 1,506 (Universities and Colleges Admissions Service, 2013). Dividing U@Uni2 roll-out costs by this figure results in a cost of £10.43 per person (£9.00 to £11.86, 95% CI).
The costs of rolling out U@Uni2 over a five year period were estimated as £4,563 per year (£3,842-£5,292, 95% CI), of which £2,946 was due to annuitized setting up costs and £1,617 was yearly maintenance costs. This was equivalent to £3.03 per student (£2.55 to £3.51, 95% CI). Comparable inflated costs for U@Uni1 were £9,434 (£8,530-£11,234, 95% CI), of which £6,069 was due to annuitized setting up costs and £3,365 was yearly maintenance costs. This worked out as £6.26 (£5.66 to £7.46, 95% CI) per person.
Within-trial cost-effectiveness analysis results
The within-trial analysis found that the U@Uni2 intervention cost an extra £35.30 (£30 to £40.51, 95% CI, based on 5000 bootstrap runs) per individual when compared with the control arm, considerably lower than the incremental costs generated in the intervention arm of the U@Uni1 trial (£326.37). The incremental cost was entirely due to the cost of the intervention, as healthcare utilization was reduced in the intervention arm of the trial, resulting in lower healthcare costs when compared with the control arm (-£10.67). Although, the intervention group used fewer healthcare resources during the 6-month trial period, they also gained fewer QALYs than the control group (-0.0025 incremental QALYs), although this was not statistically significant (0.0001 to -0.0051, 95% CI, based on 5000 bootstrap runs).
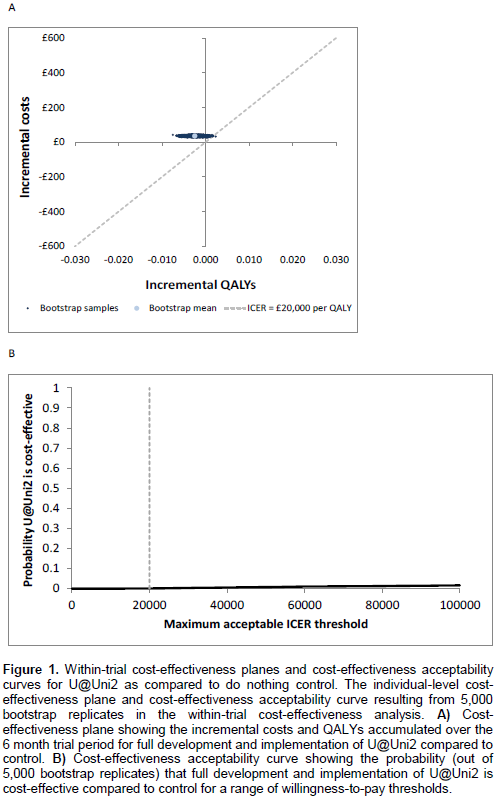
The incremental cost-effectiveness ratio (ICER) was calculated at -£14,314 per QALY gained (at a threshold of £20,000 per QALY). INB was found to be -£84.63, indicating that the intervention is not cost-effective in the short-term, due to the negative estimated QALY gain. Uncertainty analysis determined that the probability the intervention would be cost-effective at this threshold is only 0.0004 (Figure 1).
Long-term economic modelling results
The long-term lifetime economic modelling results are presented in detail in Figure 2. Both U@Uni1 and U@Uni2 produce small increases in life years and QALYs gained as compared to the control. However, U@Uni2 is slightly less effective than U@Uni1, producing only 0.00533 incremental QALYs when compared with the 0.00767 incremental QALYs produced by U@Uni1.
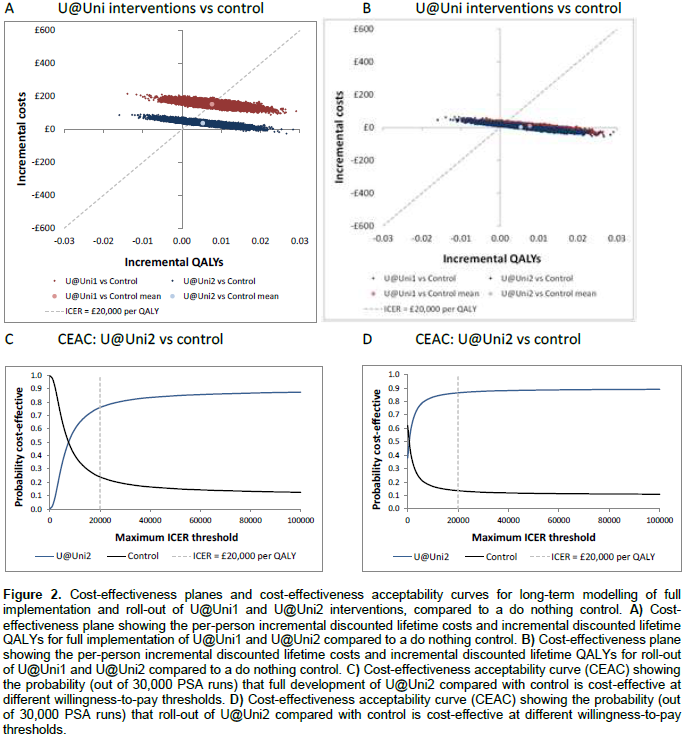
Incremental costs for full implementation of U@Uni2 when compared with control are £37.90, resulting in an ICER of £7,106, an INB of £69 and a probability cost-effective of 76% (Tables 1 and Figure 2). In contrast, incremental costs for full implementation of U@Uni1 are £152.94. The intervention is marginally cost-effective with an ICER of £19,947, but there is a high level of uncertainty around this result as the probability cost-effective is only 49%. Direct comparison indicates that the updated U@Uni2 intervention is more likely to be cost-effective than the original U@Uni1 intervention, with a probability of 75% and INB of £68 (Table 1).
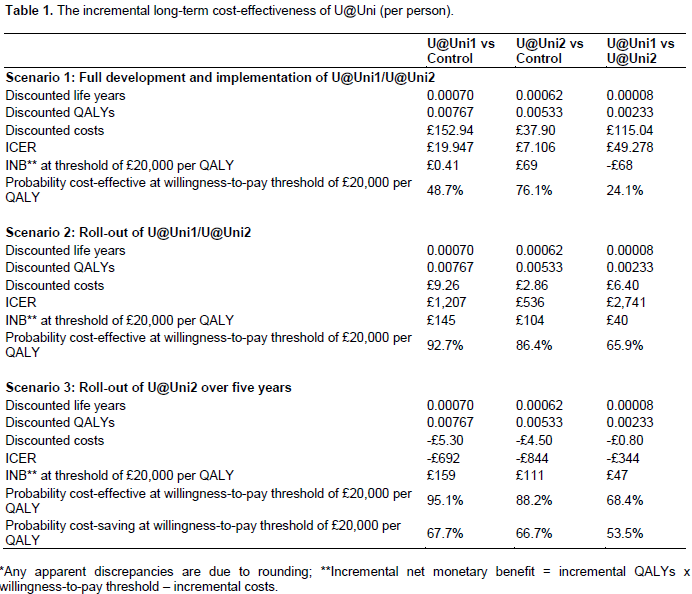
Roll-out of U@Uni2 costs only £2.86 per person, when compared with £9.26 for roll-out of U@Uni1. Both interventions are likely to be cost-effective in the roll-out scenario when compared with control to a similar extent (ICER = £1,207 for U@Uni1, probability cost-effective =93%; ICER = £536 for U@Uni2, probability cost-effective = 86%) (Table 1 and Figure 2). Despite higher costs, the net benefit gained by U@Uni1 (£144) is slightly higher than for U@Uni2 (£104), due to its larger incremental QALY gain. However, there is a high level of uncertainty around the relative cost-effectiveness of the two interventions and they occupy similar distributions on the cost-effectiveness plane (Figure 2B).
Rolling out either intervention over a five year period is estimated to be cost saving as compared to control, as the reduction in healthcare cost outweighs the cost of the interventions. £5.30 is saved per person for U@Uni1 and £4.50 is saved per person for U@Uni2. Again, both interventions are highly likely to be cost-effective when compared with control (INB of U@Uni1 = £159, probability cost-effective = 95%; INB of U@Uni2 = £111, probability cost-effective = 88%), and are cost-effective as compared to the standard roll-out from a cost-minimization perspective.
Structural sensitivity analyses
Sensitivity analyses suggest that the results are not sensitive to the removal of model updates, but they are sensitive to the method of imputation for missing data (Appendix Table 2).
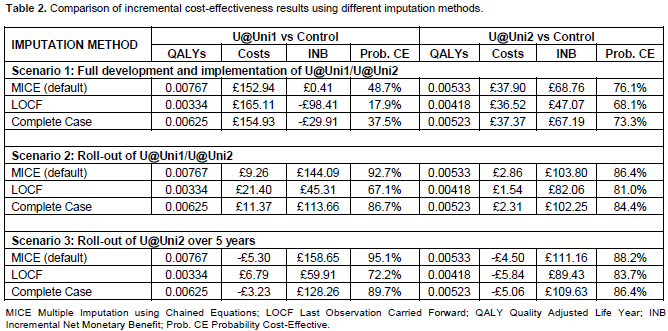
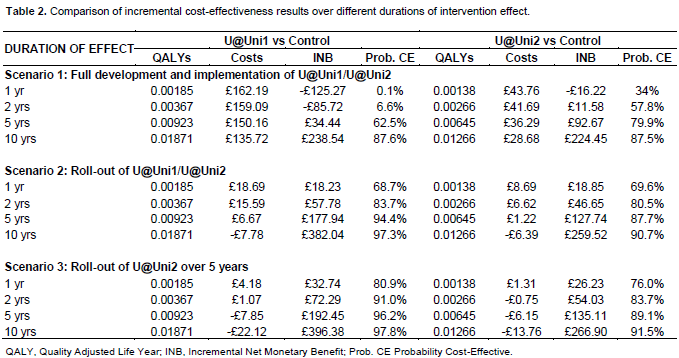
The cost-effectiveness of all scenarios is correlated with the duration of intervention effect (Table 2). For roll-out, both interventions have almost 70% probability of being cost-effective even if the mean duration of intervention effect is only 1 year, and by 10 years, both interventions are cost saving. Rollout of both interventions over 5 years is highly likely to be cost-effective in all situations, but only becomes cost-saving if duration of intervention effect lasts for about 2-3 years.
The model allows assessment of the individual contribution of each health behaviour change to quality of life and mortality. Results show that the reduction in smoking accounts for almost 75% of the incremental life years gained with U@Uni1 and over 60% of the incremental life years gained with U@Uni2. An increase in physical activity accounts for a further 20% of incremental life years gained whilst the other two behaviours contribute only very slightly to mortality reductions. The utility effects of smoking are even more dramatic than the mortality effects, such that the entire QALY gain seen in both interventions is purely due to the effect of the interventions on smoking.
Value of information
Value of information analysis was performed for roll-out of the U@Uni2 intervention versus the control only. The overall value of information from EVPI analysis was found to be £6.54 per person for the roll-out of U@Uni2. The population potentially affected by the decision was the individuals starting university each year. In 2013, there were 495,560 UCAS acceptances in the UK (Universities and Colleges Admissions Service, 2013), meaning that it could be worth spending up to £3.24 million on further research that would enable an accurate decision to be made within a year. EVPPI analysis indicates that decision uncertainty is driven primarily by the parameters relating to the effects of the intervention on health behaviours, worth up to £3.79 per person or £1.9 million in total (Table 3). The individual parameters that have by far the most influence are the rates of non-smokers taking up smoking in the U@Uni2 and control conditions, which are worth 31p and 21p per person, respectively.
The U@Uni2 intervention is an updated version of the U@Uni theory-based online health behaviour intervention for students as they start university (Cameron et al., 2015; Epton et al., 2014). This analysis shows that the U@Uni2 intervention is considerably cheaper to implement than U@Uni1. However, lifetime modelling indicates that U@Uni2 is likely to be less effective than U@Uni1, producing both fewer life years and fewer QALYs. Roll-out of U@Uni2 is highly likely to be more cost-effective than doing nothing, but is not likely to be more cost-effective than roll-out of U@Uni1.
The Life Guide software was more user-friendly than the U@Uni1 website, and this together with some changes to trial design resulted in increased levels of recruitment and engagement with the intervention (Cameron et al., 2015). Despite these changes, the U@Uni2 intervention did not show a significant improvement in any of the four behaviours and the U@Uni2 trial itself was not found to be cost-effective due to a small reduction in health-related quality-of-life. QALY loss during the trial is likely to be due to stochastic sample variability and low sensitivity of the EQ-5D to measuring subtle changes in quality of life at the top of the scale (Brazier et al., 2007).
Improvements in smoking behaviour appear to account for the vast majority of life-years and QALYs gained for both interventions. This is driven by the large effects smoking has on both quality of life and mortality compared with the other behaviours (Kruger et al., 2014; Kvaavik et al., 2010). A recent review of the economic impacts of smoking suggests that the direct costs of smoking may use 5% of the annual NHS budget, and far outweigh any economic benefits such as increased tax intake (Ekpu and Brown 2015). This suggests that specifically targeting smoking may not only be the best way to improve the health of young people, but will have positive economic consequences in the long term. In line with this, smoking cessation programmes aimed at young people have been found to be highly cost-effective in other economic analyses (Dino et al., 2008; Hollingworth et al., 2012).
A series of sensitivity analyses were carried out to test assumptions of model structure and methodology. Sensitivity analyses around the duration of intervention effect produced the largest changes in cost-effectiveness. Very little work has been done to investigate the likely duration of effect of online health interventions; this would be a useful area for further research. EVPPI analysis indicates that the highest level of decision uncertainty is around the effect of the intervention on health behaviours, particularly smoking. As intervention effectiveness is key to deciding whether to fund U@Uni2, decision makers may wish to invest in gathering more information to inform these parameters.
Taken together, the results of the two U@Uni trials suggest that online interventions can have a positive effect on health behaviours in new university students. These effects may be very small, but over a lifetime can result in significant health gains that are extremely cost-effective to implement. Similar small but positive effects have been found recently in other trials of online interventions aiming to reduce unhealthy behaviours in students (Kattelmann et al., 2014; Kypri et al., 2014). However, the U@Uni interventions remain unique amongst similar online health behaviour interventions in their demonstration of cost-effectiveness in addition to efficacy.
This study was performed from the perspective of the UK Department of Health; however, it is unclear whether they would be willing to fund such an intervention. Public health funding is concerned both with maximizing efficiency and reducing inequity (National Institute for Health and Clinical Excellence, 2012). University students are disproportionately from more privileged backgrounds (Universities and Colleges Admissions Service, 2014), and individuals with a degree have better health outcomes (Higher Education Funding Council for England, 2001) meaning that funding the U@Uni2 intervention could act to increase health inequalities. However, given the commitment of universities in England to the “Healthy Universities Scheme” to improve student health and well-being (UK National Healthy Universities Network, 2015), and the relatively low costs involved, larger universities may themselves wish to consider funding a U@Uni2 type intervention as part of their student health and well-being programme.
CONCLUSIONS AND RECOMMENDATIONS
This study estimates the costs and cost-effectiveness of U@Uni2, an updated version of the U@Uni trial of an online intervention targeting multiple health behaviours in new university students. The study shows that U@Uni type interventions are cost-effective to roll-out and suggests that universities committed to student health consider such an intervention given the low costs involved. Most of the decision uncertainty is associated with the effect of the intervention on health behaviour change, suggesting that further research should focus on this area. Given that intervention efficacy is almost entirely dependent on the smoking effect, targeting smoking is a priority for improving healthy behaviours in young people.
The authors have not declared any conflict of interests.
The authors thank Jen Kruger for her detailed notes that enabled easy adaptation of the original U@Uni model for U@Uni2. They also thank Paul Richards and Duncan Gillespie for their advice on R programming and statistical analysis. Many thanks also to Clare Relton, Annette Haywood, Amanda Loban and Mark Green for supplying first-wave data from the Yorkshire Health Study. The YHS data were managed by the University of Sheffield’s Clinical Trials Research Unit. Anonymous data and details regarding using the resource for recruiting participants to studies can be gathered by contacting Clare Relton (
[email protected]); multi-disciplinary collaboration is strongly encouraged.
The study was funded by the UK National Prevention Research Initiative (NPRI) Phase 4 (grant number: MR/J0004501/1). The NPRI includes the following Funding Partners (in alphabetical order): Alzheimer's Research Trust, Alzheimer's Society, Biotechnology and Biological Sciences Research Council, British Heart Foundation, Cancer Research UK, Chief Scientist Office, Scottish Government Health Directorate, Department of Health, Diabetes UK, Economic and Social Research Council, Health and Social Care Research and Development Division of the Public Health Agency (HSC & R&D Division), Medical Research Council, The Stroke Association, Wellcome Trust, Welsh Assembly Government and World Cancer Research Fund. This report is independent research supported (in part) by the National Institute for Health Research (Mark Strong - Post-Doctoral Fellowship, PDF-2012-05-258). The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health.
REFERENCES
|
Ajzen I (2005). Attitudes, Personality and Behaviour, 2 ed. Milton Keynes, Open University Press P 174.
|
|
|
|
Brazier J, Ratcliffe J, Salomon JA, Tsuchiya A (2007). Measuring and valuing health benefits for economic evaluation. Oxford, Oxford University Press.
|
|
|
|
|
Cameron D, Epton T, Norman P, Sheeran P, Harris PR, Webb TL, Julious SA, Brennan A, Thomas C, Petroczi A, Naughton D, Shah I (2015). A theory-based online health behaviour intervention for new university students (U@Uni:LifeGuide): results from a repeat randomized controlled trial. Trials 16(1):1.
Crossref
|
|
|
|
|
Dino G, Horn K, Abdulkadri A, Kalsekar I, Branstetter S (2008). Cost-effectiveness analysis of the Not On Tobacco programme for adolescents smoking cessation. Prevent. Sci. 9(1):38-46.
Crossref
|
|
|
|
|
Dolan P, Gudex C, Kind P, Williams A (1995). A social tariff for EuroQol: results from a UK general population survey Centre for Health Economics, University of York. Available at:
View
|
|
|
|
|
Ekpu VU, Brown AK (2015). The economic impact of smoking and reducing smoking prevalence: review of evidence. Tobacco Use Insights 8:1-35.
Crossref
|
|
|
|
|
Epton T, Norman P, Dadzie AS, Harris PR, Webb TL, Sheeran P, Julious SA, Ciravegna F, Brennan A, Meier P, Naughton D, Petroczi A, Kruger J, Shah I (2014). A theory-based online health behaviour intervention for new university students (U@Uni): results from a randomised controlled trial. BMC Pub. Health 14(1):1.
Crossref
|
|
|
|
|
Friedman HS, Martin LR, Tucker JS, Criqui MH, Kern ML, Reynolds CA (2008). Stability of physical activity across the lifespan. J.Health Psychol. 13(8):1092-104.
Crossref
|
|
|
|
|
Gollwitzer PM, Sheeran P (2006). Implementation intentions and goal achievement: A meta-analysis of effects and processes. Adv. Exp. Soc. Psychol. 38:69-119.
Crossref
|
|
|
|
|
Harris PR, Epton T (2009). The impact of self-affirmation on health cognition, health behaviour and other health-related responses: A narrative review. Soc. Personal. Psychol. Compass. 3:(6) 962-978.
Crossref
|
|
|
|
|
Higher Education Funding Council for England (2001). The Wider Benefits of Higher Education: Health and Vulnerability. Report 01/46. 2001. Available at:
View.
|
|
|
|
|
Hollingworth W, Cohen D, Hawkins J, Hughes RA, Moore LAR, Holliday JC, Audrey S, Starkey F, Campbell R (2012). Reducing smoking in adolescents: cost-effectiveness results from the cluster randomised ASSIST (A stop smoking in schools Trial). Nicotine Tob. Res. 14(2):161-168.
Crossref
|
|
|
|
|
Kattelmann KK, Bredbenner CB, White AA, Greene GG, Hoerr SL, Kidd T, Colby S, Horacek TM, Phillips BW, Koenings MM, Brown ON, Olfert MD, Shelnutt KP, Morrell JS (2014). The Effects of Young Adults Eating and Active for Health (YEAH): A Theory-Based Web-Delivered Intervention. J. Nutr. Educ. Behav. 46(6):S27-S41.
Crossref
|
|
|
|
|
Kruger J, Brennan A, Strong M, Thomas C, Norman P, Epton T (2014). The cost-effectiveness of a theory-based online health behaviour intervention for new university students: an economic evaluation. BMC Pub. Health 14(1):1.
Crossref
|
|
|
|
|
Kvaavik E, Batty GD, Urskin G, Huxley R, Gale CR (2010). Influence of individual and combined health behaviors on total and cause-specific mortality in men and women: the United Kingdom health and lifestyle survey. Arch. Int. Med. 170(8):711-718.
Crossref
|
|
|
|
|
Kypri K, Vater T, Bowe SJ, Saunders JB, Cunningham JA, Horton NJ, McCambridge J (2014). Web-Based Alcohol Screening and Brief Intervention for University Students: A Randomized Trial. J.A.M.A 311(12):1218-1224.
Crossref
|
|
|
|
|
National Institute for Health and Clinical Excellence (2012). Methods for the development of NICE public health guidance (third edition). Available at:
View.
|
|
|
|
|
Office for National Statistics (2014). Consumer Price Inflation Reference Tables.
|
|
|
|
|
Plotnikoff RC, Costigan SA, Williams RL, Hutchesson MJ, Kennedy SG, Robards SL, Allen J, Collins CE, Callister R, Germov J (2015). Effectiveness of interventions targeting physical activity, nutrition and healthy weight for university and college students: a systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 12(1):1.
Crossref
|
|
|
|
|
Strong M, Breeze P, Thomas C, Brennan A (2014). Sheffield Accelerated Value of Information (SAVI). University of Sheffield. Available at:
View.
|
|
|
|
|
The King's Fund (2014). Time to Think Differently: Trends in Health Behaviours.
|
|
|
|
|
UK National Healthy Universities Network (2015). Healthy Universities. Available at:
View.
|
|
|
|
|
Universities and Colleges Admissions Service (2014). UCAS Free School Meal Application Rates. Available at:
View
|
|
|
|
|
White IR, Royston P, Wood AM (2011). Multiple imputation using chained equations: Issues and guidance for practice. Stat. Med. 30(4):377-99.
Crossref
|
|
|
|
|
Yang Y, Osmond A, Chen X, Weal M, Wills G, De Roure D, Joseph J, Yardley L (2009). Supporting the running and analysis of trials of web-based behavioural interventions: the LifeGuide. Ine-Science, 2009. e-Science'09. Fifth IEEE International Conference IEEE. pp. 50-57.
Crossref
|
|