ABSTRACT
Neonatal tetanus (NNT) is still one of the major preventable causes of neonatal death in Nigeria. It is a disease of poverty, adverse social and environmental conditions. The aim of the study was to review neonatal tetanus cases, determine the prevalence, disease outcome and what possible interventions can be done in the study area to reduce its prevalence. This was a retrospective study of cases of NNT seen in Special Care Baby Unit of Ahmadu Bello University Teaching Hospital, Zaria, Nigeria from 2001 to 2014. Case notes of neonates with clinical diagnosis of tetanus who were admitted into the unit were retrieved for analysis. Data extracted included: socio-demographic characteristics, antenatal clinic (ANC) history, TT immunization, place of delivery and disease outcome. There were a total of 60 cases of NNT during the period; this gave an annual prevalence of 4.3 per year. Mean age of neonates was 9.3 ± 5.1 days, M: F ratio was 4.0:1.0. Mean age of mothers was 23.2 ± 4.0 years, majority (55%) had no formal education, 48% had ≤ 2 ANC visits, and more than 70% had no TT immunization and delivered at home. Commonest probable portal of entry of infection was umbilicus (70%) and major presenting symptoms/signs were: spasms (81.7%), poor suckling (81.7%), inability to open mouth (45%) and fever 45%, respectively. Site of infection and presence of fever were associated poor outcome. Mortality among neonates who had short incubation period (≤ 6 days), umbilicus as probable site of infection (P=0.006) and presence of fever (P=0.014) were significantly higher for non-survivors than survivors. Overall, case fatality rate (CFR) was 56.7%. The review revealed that CFR is still unacceptably high for a disease that can be prevented and eventually eliminated with cost effective and affordable public health interventions. All the 3 tiers of government need to re-focus the National Immunization Policy together with sustained immunization programmes throughout all the communities in Nigeria. There is urgent need for health education at community level on the importance of ANC and mass immunization regardless of age in order to achieve the goal of NNT elimination.
Key words: Neonatal tetanus (NNT), immunization, prevention, tertiary hospital, Nigeria.
Tetanus is a disease characterised by muscle rigidity and spasms and was first described in Egypt over 3000 years ago. Clostridium tetani that causes tetanus is a ubiquitous strictly anaerobic Gram positive bacillus that is present in the soil and in human and animal faeces. It is a disease that is largely now confined to developing countries. Efforts by World Health Organization (WHO) to eradicate the disease by 1995 has not yielded any remarkable success as tetanus still remains one of the world’s major preventable causes of mortality with an estimated incidence of 700,000 to 1 million cases a year, causing an estimated 213, 000 death (World Health Organization, 2006; Thwaites and Farrar, 2003). In 1890, Faber discovered tetanus toxin and in the same year, von Berhring and Kitasario produced the first antitoxin. In 1926, Raman performed the first successful vaccination in humans (Catherine and Lam, 2009). Tetanus is a positive environmental hazard and its occurrence depends upon man’s physical and ecological surroundings [soil, Agriculture and animal husbandry] and not on the presence or absence of infection in the population. Thus, C. tetani will never be eradicated from the soil and so wherever vaccination programmes are ineffective and or inadequate, tetanus will continue to occur. In 2004, an estimated 27 million children did not complete their immunization (World Health Organization, 2006). Neonatal tetanus (NNT) usually arises from contamination of umbilical cord, unhygienic delivery practices, traditional midwifery practices (cutting the umbilical cord with dirty blade, bamboo, applying soil, cow dung, hot fermentation and charcoal or even engine oil to the umbilical stump). Gitta et al. (2006) and Alhaji et al. (2013) Ritual surgery (ear piercing) or circumcision, uvelectomy may also cause infection (Charles, 2004). Another source of infection is otitis media (Catherine and Lam, 2009; Charles, 2004).
Neonatal tetanus [NNT] can be prevented by maternal immunization, yet in 2004, WHO estimated that about 40 million pregnant women were unimmunized (World Health Organization (WHO) (2006). Tetanus elimination needs continuing vaccination programmes because the tetanus spores are widespread in soil and faeces throughout the world. Vaccination is started at two months of age with 3 injections performed at monthly intervals (Cook et al., 2001) and a second injection confers immunity (Ruben et al., 1973) with a third prolonging its duration. A booster dose is given before the age of five years. Immunity is not life long, so revaccination is recommended at 10 year intervals in adulthood. Neonatal immunity is provided by maternal vaccination and transplacental transfer of immunoglobulins. It has been reported that even after maternal immunization, the infant is still at risk of infection as malaria and HIV infections reduce placental transfer of protective antibodies (Brair et al., 1994; de Moraes-Pinto et al., 1996) In Africa, neonates account for up to 40% of the patients admitted to hospital with tetanus in some areas and they tend to have the highest mortality rates. Furthermore, it was reported that mortality rates varied between 0.3/1000 live births in Egypt to 15.0/1000 live births in Somalia (Charles, 2004). The incidence of neonatal tetanus in Nigeria ranges between 14.6 and 20.0 per 1000 live births (Federal Ministry of Health and Human Services (FMOH & HS), Nigeria (1992), it contributes 16% to the global neonatal deaths UNICEF/WHO/UNFPA (2005). Without medical care, mortality from NNT is close to 100% and often exceeding 50% with hospital care (Louise et al., 2014; Roper et al., 2007; Black et al., 2010). Thus, the elimination of maternal and neonatal tetanus is a key area in global public health policy as maternal immunization has resulted in 82% of today’s newborn babies being protected from tetanus UNICEF (2013) Most countries in sub-Saharan Africa (SSA) including Nigeria are undergoing demographic transition with a very young population and with more women in reproductive age group Cincotta (2010). Nigeria is still among the countries that is yet to achieve the WHO goal to eliminate neonatal tetanus (defined as; less than one case per 1000 live births in every district of every country) UNICEF/WHO/UNFPA (2005) The study aimed to review neonatal tetanus cases, determine the prevalence, disease outcome and what possible interventions can be done in the study area to decrease its prevalence. The paucity of literature on NNT in the study area also prompted this review.
Retrospective study of NNT patients admitted to the Special Baby Care Unit (SBCU), Ahmadu Bello University Teaching Hospital (ABUTH), Zaria over a period of 14 years (2001-2014) was conducted. The teaching hospital was established in 1967 to serve as a referral centre for the former Northern region, located in North western part of Nigeria. Currently, it has 21 clinical departments as well as being centre of excellence in oncology. The medical records (case notes/folders) of all the cases during the period were retrieved and reviewed. Relevant data extracted for this study came from the case notes (folders) of the patients and included socio-demographic characteristics of mothers of patients, age of neonate at the time of admission, focus/site of infection, clinical signs and symptoms at presentation, antenatal care history of mothers, history of tetanus toxoid [TT] immunization of mothers and place of delivery. The criteria for diagnosis was based on clinical findings; muscle spasms, inability to suck, trismus and has been used in previous studies (Bunyamin et al., 2008; Barlow et al., 2001).Data was first entered into Excel then imported into Stata13 for statistical analysis. The data was analysed by generating frequencies of cases against socio-demographic and clinical characteristics and then comparison between survivors and non-survivors. Therefore, we generated frequencies, means, standard deviations, Student’s t-test, X2-test and probit regression model since the sample size is small. This strategy avoids inflated standard errors associated with odds ratio when applying logistic regression. Furthermore, both models provide similar results but the estimates are much inflated in logistic regression as compared to probit regression (Hahn Soyer, 2005). Results are presented using appropriate tables and test of significance was done with p- value at <0.05 taken as significant.
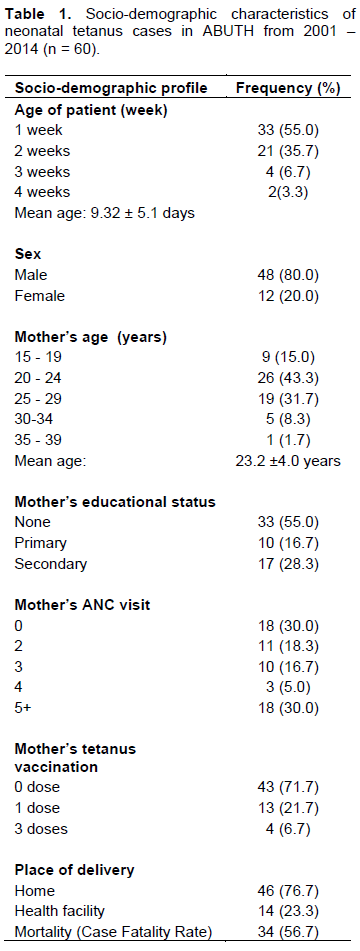
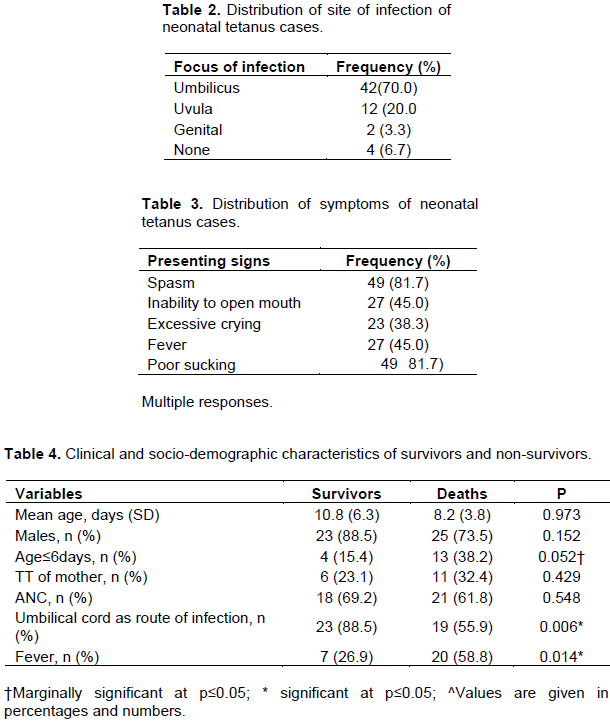
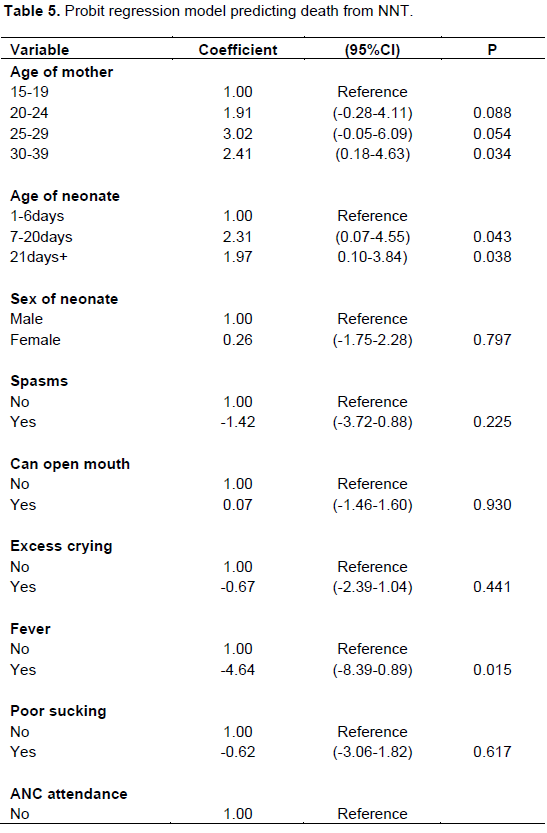
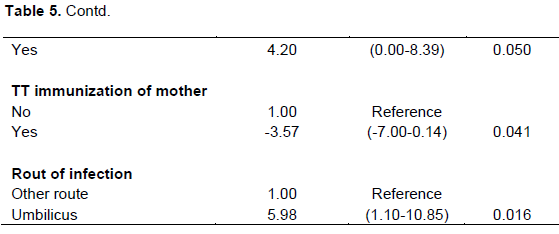
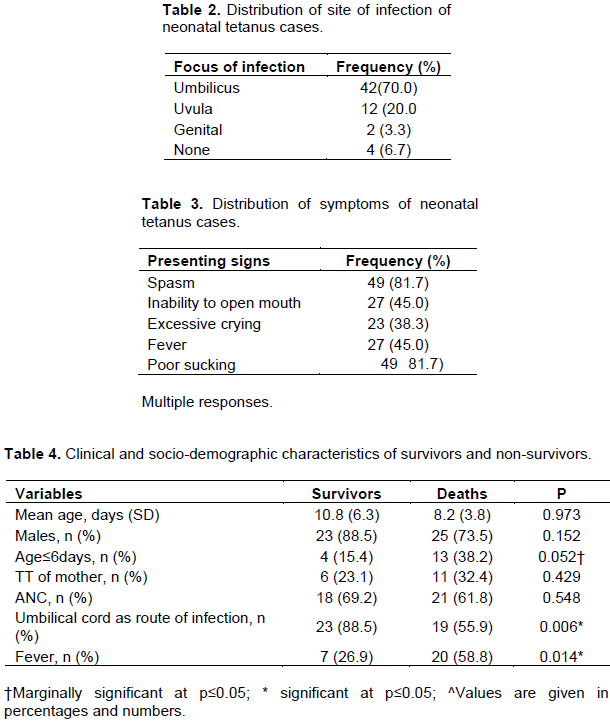
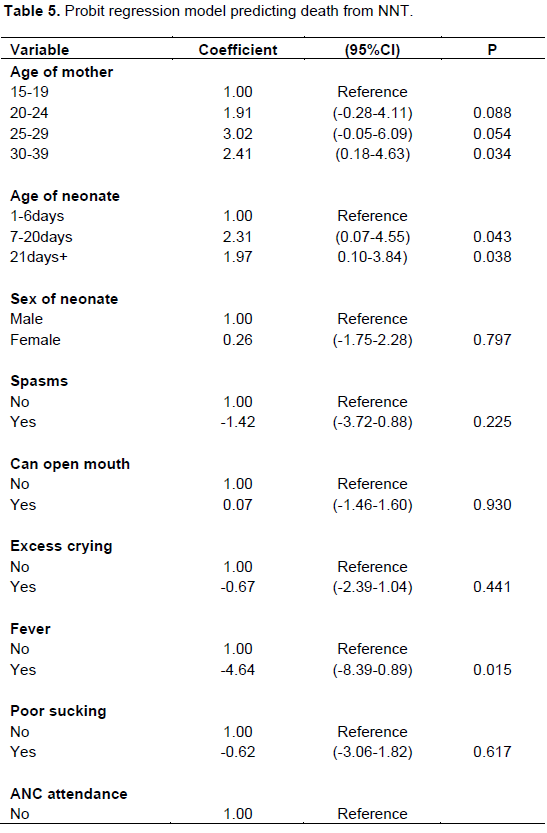
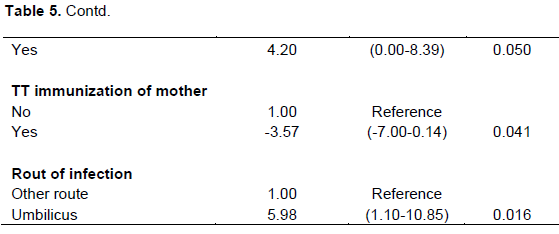
During the period under review, there were a total of 60 of NNT cases, this gave an annual prevalence of 4.3 per year. Mean age of cases was 9.3 ± 5.1 days, majority (80%) were males with M : F ratio of 4.0:1.0. Mean age of mothers was 23.2 ± 4 years, majority had no formal education (55.0%), 48.0% had ≤ 2 ANC visits, more than 70% had no TT immunization and also delivered at home assisted by relatives in unhygienic environment or traditional birth attendants (TBAs) and only 23.3% delivered at health facility respectively (Table 1). The commonest probable sites of infection among cases were umbilicus 70.0%, uvula 20% and genitals 3.3%, while in 6.7%, no site was identifiable (Table 2). Major presenting symptoms/signs were respectively spasms (81.7%), poor suckling (81.7%), inability to open mouth (45%), fever (45.0%) and excessive crying (38.3%) (Table 3). Table 4 shows comparison of the values of selected variables for survivors and non-survivors; mortality among neonates who had short incubation period (≤ 6 days), umbilicus as probable site of infection (P=0.006) and presence of fever (P=0.014) were significantly higher for non-survivors than survivors. Mortality was not significantly higher with age, mothers’ TT status and ANC attendance. Probit regression model was used to determine the effects of mothers’ age, age of neonate, ANC attendance, TT immunization status of mothers, etc on mortality (Table 5). The result revealed that route of infection (umbilicus) significantly increases the risk of mortality several folds (six times) while TT immunization was protective. Finally, from a total of 60 cases, 26 (43.3%) survived while 34 cases died, giving an overall case fatality rate (CFR) of 56.7%.
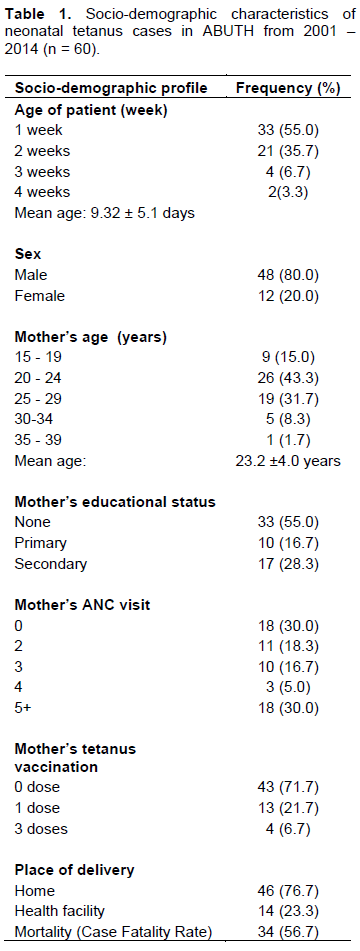
The neonatal period is only 28 days, yet accounts for 38% of all deaths in children younger than 5 years of age and globally some three-quarter of neonatal deaths occur in the first week after birth Joy et al., 2005; Zupan and Aahman, 2005). Mortality from NNT still remains high, despite being preventable using affordable and accessible public health measures. There were a total of 60 cases over the review period with an annual prevalence of 4.3 per year. This prevalence is still unacceptably high particularly in the 21st century as Nigeria has all the resources needed to meet the WHO maternal and neonatal tetanus elimination by 2005, almost a decade ago.
The results of univariate analyses shows that survival is significantly associated with site of infection (cord) and presence of fever, but is not associated with age, infant’s sex, TT immunization of mothers or ANC attendance. The findings relating to ANC and place of delivery (home) are well known and widely accepted. But these factors were not significant in regression model which again showed route of infection (umbilicus) as the most consistent and strongest predictor for non-survival. The most probable explanation for these are that poor home delivery environment as well as harmful traditional cord care practices are all conditions that predispose to cord sepsis and fever. This is consistent with earlier studies (Alhaji et al., 2013; Ambe et al., 2009; Abhulimenhen-Ihoha et al., 2011). The fever may be as a result of sepsis from the infected site and or secondary bacterial infection arising from unhygienic practices which will further worsen the clinical condition of the patients and resulting in high mortality. It is important therefore, for policy makers to promote and encourage hygienic midwifery, umbilical cord care and delivery services.
TT immunization status of mothers was found not to be significant in this study in agreement with previous study (Anita et al., 1998) but in contrast to many local and international studies (Anita et al., 1998; Onalo et al., 2011; Mbarie and Abhulimhen-Iyoha, 2015; Bunyamin et al., 2008). Studies have shown that many factors can potentially confound the protective efficacy of TT which include; ineffective immune response, defective transfer of protective antibodies across the placenta especially among African women (Hlady et al., 1992) and quality problems associated with vaccine production (Anita et al. 1998). Importantly, the erratic power supply coupled with incessant power outrages resulting in inefficient cold chains which is common in Nigeria can reduce the efficacy and potency of vaccine. Thus, to ensure efficiency of vaccines, health care facilities need to be provided with alternative source of power/electricity such as the use of solar panels.
In this study, the umbilicus was identified as the probable portal of entry in two-thirds of cases followed by uvula in a third of cases. This is consistent with report of other studies with local practices of cutting the cord with potentially infectious instruments (Alhaji et al., 2013; Onalo et al., 2011; Mbarie and Abhulimhen-Iyoha, 2015). It is also a traditional practice to perform uvulectomy conducted by “local surgeons” using unsterile tools in the study area (Onalo et al., 2011) on the new born within the first seven days of birth. The continued persistence of these practices will mean persistence of NNT in the study community and indeed Nigeria and thus require urgent sustained public health interventions (health education, community mobilization) on hygienic delivery and post delivery cord care to prevent these practices.
A recent report in Nigeria (National Population Commission (NPC) Nigeria and ICF International 2014) revealed that 61% of pregnant women had ANC, 51% had at least 4 ANC visits, 53% of them had protection against neonatal tetanus and only 36% had health facility delivery respectively. In this study, more than 70% of mothers had no TT immunization and only 48% had at least 2 ANC visits. Added to these factors is the fact that majority of the mothers (70.6%) delivered at home which is in agreement with the report of an earlier study (Joy et al. 2005). Again, the need to make health care accessible and affordable in order to encourage utilization of health care services cannot be over emphasized. This will go along way in reducing neonatal tetanus incidence and mortality not only in the study area but Nigeria as a whole.
The case fatality rate (CFR) of 56.7% reported in this study is comparable to the findings of several studies in Nigeria and elsewhere (Alhaji et al., 2013; Onalo et al., 2011; Ogunlesi et al., 2007; Yaramis and Tas, 2000). Eliminating NNT is possible and achievable in our communities using cost effective public health measures. That is why it is regarded as one of the simplest and most cost effective way to reduce neonatal mortality rate (Joy et al., 2005; Ertem et al., 2004). Immunization of pregnant women or women of childbearing age with 2 doses of TT was estimated to reduce mortality from NNT by 94.0% (Biencave et al., 2010). Thus, all tiers of government need to re-focus the implementation of National Immunization Policy which recommends five doses of TT for women of childbearing age (National Immunization Policy, 2009). Furthermore, there is need for community-wide publicity campaigns on the importance and benefits of ANC for pregnant mothers in order to increase its acceptance and utilization. Health education to TBAs, elderly women who care for pregnant women during delivery and their babies on hygienic practices is of utmost importance.
CONCLUSION AND RECOMMENDATION
Prevention and eventual elimination of NNT in our community is possible if there is political will to harness the resources to use public health measures- intensive, sustained, periodic health education through the mass media on cord care and health facility delivery, mass immunization campaigns starting at the grassroots regardless of age and community mobilization.
Study limitation
There was slightly higher percentage of males than females which may be due to gender bias in care seeking. The findings may also not reflect the true prevalence of the disease in the study area because of “iceberg phenomenon” whereby only the most serious cases are brought to the health facility. As reported by WHO, there is the issue of under-reporting of neonatal tetanus cases which are influenced by performance and reporting artefacts (WHO, 2004). The problem of proper record keeping in this part of the world has to be borne in mind, it is possible some case notes/folders were not captured by us and thus not included in the study.
The authors have not declared any conflict of interests.
REFERENCES
|
Abhulimenhen-Ihoha BI, Ofili A, Ibadin MO (2011). Cord care practices among mothers attending immunization clinic at University of Benin Teaching Hospital, Benin City. Niger. J. Paediatr. 38:104-108.
|
|
|
|
Anita A, Davies-Adetugbo, Torimoro SEA, Ako-Nai KA (1998). Prognostic factors in neonatal tetanus. Trop. Med. Int. Health 3(1):9-13.
Crossref
|
|
|
|
|
Ambe JP, Bello M, Yahya SJ, Omotara BA (2009). Umbilical cord care practices in Konduga LGA of Borno state, North east Nigeria. Int. J. Trop. Med. P 5.
|
|
|
|
|
Alhaji MA, Bello MA, Elechi HA, Akuhwa RT, Bukar FL, Ibrahim HA (2013). A review of Neonatal tetanus in University of Maiduguri Teaching Hospital, North eastern Nigeria. Niger. Med. J. 54(6):398-401.
Crossref
|
|
|
|
|
Barlow JL, Mung'ala-Odera V, Gona J, Newton CRJC (2001). Brain damage after neonatal tetanus in rural Kenyan hospital. Trop. Med. Int. Health 6(4):305-308.
Crossref
|
|
|
|
|
Biencave H, Lawn J, Vandelaer J, Roper M, Cousens S (2010). Tetanus toxoid immunization to reduce mortality from Neonatal tetanus. Int. J. Epidemiol. 39(sppl 1):1102-1109.
|
|
|
|
|
Black RE, Cousens S, Johnson HL, Lawn JE, Rudan I, Bassani DG, Eisele T (2010). Global, Regional and National causes of child mortality in 2008: a systematic analysis-The Child Health Epidemiology Reference Group of WHO and UNICEF. Lancet 375(9730):1969-1987.
Crossref
|
|
|
|
|
Brair ME, Brabin BJ, Milligan P, Maxwell S, Hart CA (1994). Reduced transfer of tetanus antibodies with placental Malaria. Lancet 343:208-209.
Crossref
|
|
|
|
|
Bunyamin D, Hakan U, Ebru YK, Taskin T, Ali G, Halal K, Tas MA (2008). Neonatal tetanus in Turkey: what has changed in the last decade. BMC Infect. Dis. 8(1):112.
Crossref
|
|
|
|
|
Catherine LT, Lam MY (2009). Tetanus, In: Gordon C Cook and Alimuddin I Zumla (Eds). Manson's Tropical Diseases 22nd Edition, China, Saunders Elsevier. pp 1113-1118.
|
|
|
|
|
Charles RJC (2004). Tetanus, In Principles of Medicine in Africa (Eldryd Parry, Richard Godfrey, David Mabey and Geoffrey Gill, eds). Cambridge University press UK.
|
|
|
|
|
Cincotta R (2010). The future of SSA's tentative fertility decline.
|
|
|
|
|
Cook TM, Protheroe RT, Handel JM (2001). Tetanus: a review of literature. Br. J. Anaesth. 87:477-487
Crossref
|
|
|
|
|
Cvetanovic B (1978). Dynamics of acute bacterial diseases: epidemiological models and their applications in Public Health: part II. Epidemiological models of bacterial diseases. Bull. World Health Org. 1:29.
|
|
|
|
|
de Moraes-Pinto MI, Almeida AC, Kenj G (1996). Placental transfer of maternal acquired neonatal IgG immunity in human immunodeficiency virus infection. J. Infect. Dis. 173(5):1077-1084.
Crossref
|
|
|
|
|
Ertem M, Cakmak A, Saka G, Ceylan A (2004). Neonatal tetanus in the South-Eastern region of Turkey: changes in prognostic aspects by better health care. J. Trop. Pediatr. 50:297-300.
Crossref
|
|
|
|
|
Federal Ministry of Health and Human Services (FMOH & HS), Nigeria (1992). Neonatal tetanus. Niger. Bull. Epidemiol. 2:13-16.
|
|
|
|
|
Fetuga BM, Ogunlesi TA, Adekanmbi FA (2010). Risk factors for mortality in neonatal tetanus: A 15 year experience in Sagamu, Nigeria. World J. Pediatr. 6:71-75.
Crossref
|
|
|
|
|
Gitta, Sheba N, Wabwire-Mangen F, Kitimbo D, Pariyo G (2006). "Risk factors for neonatal tetanus--Busoga region, Uganda, 2002-2003." MMWR Morb Mortal Wkly Rep. 55(Suppl 1):25-30.
|
|
|
|
|
Hahn ED, Soyer R (2005). Probit and Logit Models: differences in Multivariate Realm. J. Royal Stat. Soc. pp. 1-12.
|
|
|
|
|
Hlady WG, Bennett JV, Samadi AR, Begum J, Hafez A, Tafdar AI, Boring JR (1992). Neonatal tetanus in Bangladesh: Risk factors and toxoid efficacy. Am. J. Publ. Health 82:1365-1369
Crossref
|
|
|
|
|
Joy EL, Simon C, Jelka Z (2005). 4 million deaths: When? Where? Why? Lancet 365:891-900.
Crossref
|
|
|
|
|
Louise TC, Nicholas JB, Charles RN (2014). Maternal and neonatal tetanus. Lancet 385(9965):662-670.
|
|
|
|
|
Mbarie IA, Abhulimhen-Iyoha BI (2015). A 6 year review of Neonatal tetanus at the Stella Obasanjo hospital, Benin City, South south Nigeria. Afr. J. Med. Health Sci.14:52-55.
Crossref
|
|
|
|
|
National Population Commission (NPC) Nigeria and ICF International (2014). Nigeria Demographic and Health Survey 2013, Abuja-Nigeria and R M, USA, NPC and ICF International.
|
|
|
|
|
National Immunization Policy (2009). National Primary Health Care Development Agency. (Accessed on 3/04/2016) FMOH, Nigeria.
|
|
|
|
|
Ogunlesi TA, Okeniyi JA, Owa JA, Oyedeji GA (2007). Neonatal tetanus at the close of 20th century in Nigeria. Trop. Doct. 37:165-167.
Crossref
|
|
|
|
|
Onalo R, Ishiaku HM, Ogala WN (2011). Prevalence and outcome of Neonatal tetanus in Zaria, North western Nigeria. J. Info. Dev. Countries 5(4):255-259.
|
|
|
|
|
Roper MH, Vandelaer JH, Gasse FL (2007). Maternal and Neonatal tetanus (2007). Lancet 370:1947-1959.
Crossref
|
|
|
|
|
Ruben FL, Smith EA, Foster SO, Casey HL, Pifer JM, Wallace RB, Atta AI, Jones WL, Arnold RB, Teller BE, Shaikh ZQ (1973). Simultaneous administration of smallpox, measles, yellow fever, and diphtheria—pertussis-tetanus antigens to Nigerian children. Bull. World Health Org. 48(2):175.
|
|
|
|
|
Thwaites CL, Farrar JJ (2003). Preventing tetanus. Br. Med J. 326(7381):117-118.
Crossref
|
|
|
|
|
UNICEF/WHO/UNFPA (2005). Maternal and neonatal tetanus elimination by 2005. Strategies to achieving and maintaining elimination. (Accessed 3/5/016). WHO, Geneva. WHO.
View
|
|
|
|
|
UNICEF (2013). The state of world's children 2013. Available at: http://www.unicef.org/sowe2013.
|
|
|
|
|
WHO (2004). WHO Vaccine preventable diseases (2004): Monitoring system- 2004 global summary, WHO, Geneva.
|
|
|
|
|
World Health Organization (WHO) (2006). Tetanus vaccination Weekly. Epidemiol. Rec. 81(20):198-208.
|
|
|
|
|
Yaramis A, Tas MA (2000). Neonatal tetanus in the south east Turkey: Risk factors and clinical and prognostic aspects. Review of 73 cases, 1990-1999. Turk. J. Pediatr. 42:272-274.
|
|
|
|
|
Zupan J, Aahman E (2005). Perinatal mortality for the year 2000, estimates developed by WHO Geneva. World Health Organization.
|
|