ABSTRACT
Benign prostatic hyperplasia (BPH) is an enlarged prostate gland caused by progressive hyperplasia of glandular cells or stoma cells from prostate tissues. BPH is a common problem that increases in people from 40 years old. The symptom is lower urinary tract symptoms (LUTS) that consist of the followings: Strenuous urination, frequent urination, urinary hesitancy and retention. This study aims to know the characteristic of BPH patients in RSU Haji Medan from January to December 2015. Research design of this study is descriptive studies. The population of the study consists of patients who were diagnosed with BPH in RSU Haji Medan from January to December 2015. Total sampling method was used. Research data were retrieved by taking the patients’ entire medical record with BPH in RSU Haji Medan from January to December 2015. 84 persons were diagnosed with BPH. The highest age group of the population is 60 to 70 years (34 people (40.5%). The most common complaint of the patients with BPH is the inability to urinate (42 people (50.0%). Common volume size of prostate is 40 to 60 g (people (38.1%). The most common therapy is transurethral resection of the prostate (TURP) (people (76.2%). The highest co morbidity is hypertension (20 people (23.8%). The patients that had BPH most in RSU Haji Medan were 60 to 70 years old; the chief complaint is not being able to urinate; common size of prostate volume is 40 to 60 g; the most common therapy that is used is TURP, and the highest co morbidity is hypertension.
Key words: Benign prostatic hyperplasia (BPH), older group, transurethral resection of the prostate (TURP), hypertension.
Benign prostatic hyperplasia (BPH) is a benign enlargement of the prostate gland due to progressive glandular cells or cells of the prostate tissue stoma. BPH is the most common disorder experienced by men of over 40 years old (Purnomo, 2011; Arif, 2007; Glina and Felipe, 2013). BPH would be a clinical condition if there are varieties of symptoms in patients. These symptoms are known as lower urinary tract symptoms (LUTS) consisting of urinary symptoms (voiding symptoms) as follows: strenuous, repetitive urination, weak emission of urine and imperfect emptying of the bladder. It is also accompanied by symptoms of urinary retention (storage symptoms) urgency, frequency and nocturia (Arif, 2007). Although it in the urinary tract; he or she would often expel urine especially at night, and sometimes the urine cannot be held back. Disruption of the flow of urine would cause bacteria to easily replicate and stick to urotelium (Purnomo, 2011).
Factors affecting BPH is the background conditions of patients such as age, family history, obesity, increased blood cholesterol, a diet high in animal fat, exercise, smoking, alcohol, diabetes mellitus and sexual activity. The influence of age and prostate volume on symptom scores shows that there is a significant relationship between BPH and age (p <0.0001) (Presti, 2016). Complications that occur in patients with BPH if not treated include trabeculation that is, the thickening of detrusor fiber due to very high intra- vesical pressure caused by obstruction and also the mucosa jar that comes out between detrusor fiber. If the saturation is enlarged, it would become a diverticle. Another complication is the formation of bladder stones from the accumulation of urine residue in jars. In Surakarta, there are 14 out of 15 BPH patients with a prostate volume of more than 20 cc that have residual urine, one of the factors that cause the formation of stones in the bladder (Presti et al., 2008).
The world’s estimated number of BPH patients is as much as 30 million. In the United States, there are more than 50% ofmen aged 60 to 70 years experiencing BPH, and between the ages of 70 to 90 (90%) experience symptoms of BPH (Presti et al., 2008). In Asia, the prevalence of BPH increases from the age group 40 to 49 years, 50 to 59 years and 60 to 69 years (18%, 29% and 40% respectively).6,7 In Indonesia alone, there has been no definite incidence; but it was prevalent at two major hospitals in Jakarta, the RSCM and Sources Sane (1994-1997), with 1040 cases (Association of Indonesia’s Urologists, 2009). Patients with mild symptoms (for example, IPSS <7) should be counselled to modify their lifestyle and be watchful.
Patients with mild and bothersome symptoms should undergo further assessment. Treatment options for patients with bothersome, moderate (for example, IPSS 8 to 18) and severe (for example, IPSS 19 to 35) symptoms of BPH include to be watchful and modification of lifestyle, as well as medical, minimally invasive or surgical therapies (Rizki, 2010). The same thing also happened in RSU Haji. The standard of treatment performed is dependent on the severity of the disease and most patients receive surgical treatment. Based on literature studies conducted, researchers found no studies examining the characteristics of benign prostatic hyperplasia patients in Medan. Therefore, the researchers of this work were interested in conducting research on the characteristics of BPH patients in RSU Haji Medan from January to December 2015.
This research is a descriptive study that aims to determine the characteristics of patients with BPH in RSU Haji Medan, from January to December 2015.
Time and place of research
This study was conducted from April to December 2016 in RSU Haji Medan with BPH sample data.
Population and sample
The population of the study was all patients with BPH diagnosed in RSU Haji Medan, 2015. Research samples were data from patients with BPH; the data were taken from medical record in Haji Hospital Medan from January to December 2015. Total sampling was done for the patients with BPH in RSU Haji Medan from January to December 2015.
Inclusion criteria
(1) Patients diagnosed with BPH in medical records at RSU Haji Medan from January to December 2015.
(2) Complete medical record data (age, main complaint, the size of the prostate volume of ultrasound results, the therapy carried and co morbidities).
Exclusion criteria
(1) Patients with clinical and ultrasound results tending towards prostate cancer.
(2) Having done surgery for BPH.
Data collection technique
Data collection was performed by taking secondary data of sufferers of BPH obtained from medical records of RSU Haji Medan, from January to December 2015.
Data processing
The data processing was done through the following stages:
(1) Editing
(2) Coding
(3) Data entry
(4) Cleaning
(5) Tabulation
Data analysis
All data collected were processed and prepared in a frequency distribution table. Statistical test was done using computer application.
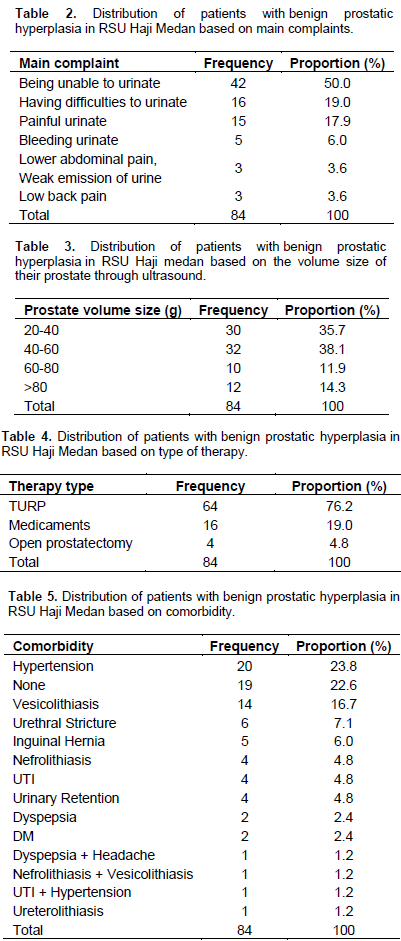
In Table 1, it is found that the highest numbers of people with BPH disease are those in the age group of 60 to 70 years (34 people (40.5%), followed by the age group of 70 to 80 years (32 people (38.1%)), the age group of 50 to 60 years (9 people ( 10.7%)), and the age group of 80 and above years (8 (9.5%)); the lowest age group is 40 to 50 years (1 person (1.2%)). In Table 2, it is found that the complaints most perceived by BPH patients include: inability to urinate (42 people (50.0%), difficulties in urinating (16 people (19.0%)), painful urination (15 people (17.9%)), bleeding urination (5 people (6.0%)); the lowest include: lower abdominal pain, weak urine emission and back pain (3 persons each (3.6%)). In Table 3, it is found that the prostate volume size observed by the sonogram is 40 to 60 (32 people (38.1%)), followed by 20 to 40 g (30 people (35.7%)), and 80 g (12 people (14.3%)); the lowest is 60 to 80 g (10 people (11.9%)). In Table 4, it is found that the therapies conducted most are: TURP (64 people (76.2%), followed by medicament (16 people (19.0%); the lowest is open prostatectomy (4 people (4.8%). In Table 5 it is found that the mostly found co morbidity is hypertension in as many as 20 people (23.8%).
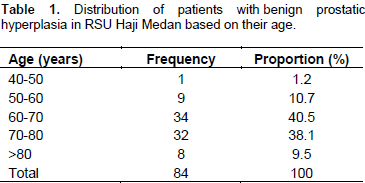
From previous research findings, it is known that the highest numbers of people with BPH disease are those in the age group of 60 to 70 years (34 people (40.5%). Amalia (2010) also found that BPH patients are mostly within the age group of 60 to 69 years (44.2% (23 people) (Amalia, 2010). Lower urinary tract symptoms (LUTS) represent one of the most common clinical complaints in adult men. The prevalence of LUTS increases with age (Gravas et al., 2015; Fjellestad-Paulsen, 1993; Rembratt et al., 2004). The major complaint found is not being able to urinate (42 people (50.0%). The obstruction caused by BPH is not only caused by the presence of prostate masses that clog the posterior urethra, but also due to the existing smooth muscle tone in the prostate stoma, prostatic capsule and smooth muscle of the bladder neck. If these conditions continue to occur then it is possible that there would be clogging of the lumen of the urethra, making the patient unable to urinate and will ultimately result in hydroureter, hydronephrosis, and consequently renal failure (Purnomo, 2011).
The prostate volume size is mostly 40 to 60 grams (32 people (38.1%)). The increasing size of the prostate volume depends on the underlying cause. One of them is the abnormal growth (hyperplasia) of the prostate that may be caused by local growth factors or the abnormal growth factor receptors, leading to increased proliferation or decreased cell death (apoptosis) (Tanagho, 2008). The most widely performed type of therapy is TURP (64 people (76.2%). This result is supported by Roar (2015) study which showed that most patients with BPH underwent the TURP therapy and most frequently at the age of 73 to 77 years (24.6%) (Roar, 2015). Monopolar TURP remains the golden standard treatment for patients with bothersome, moderate or severe LUTS who request active treatment or who either fail or do not want medical therapy (Roar, 2015; Nickel et al., 2010; Hindley et al., 2001; Madersbacher et al., 2000; Roehrborn et al., 2007; Vesely et al., 2006; Fowler et al., 2005).
Bipolar TURP has evolved as an equivalent alternative to monopolar technique. Recent reports suggest bipolar resection is associated with a reduction in the risk of dilutional hyponatremia (TUR syndrome), improvements in intraoperative visibility and may result in shorter catheterization times (Nickel et al., 2010). The most co- morbidity is hypertension (20 people (23.8%). This is supported by Kuspriyanti (2015) research which showed that most of BPH patients having elevated blood pressure in hypertension group amounted to 46.52% (Kuspriyanti, 2015). From this study we can conclude that the highest number of people with BPH disease is in the age group of 60-70 years (34 people (40.5%); the major complaint is inability to urinate (42 people (50.0%); the prostate volume size is mostly 40 to 60 grams (32 people (38.1%)); the most widely performed type of therapy is TURP (64 people (76.2%)); the most co morbidity is hypertension ( 20 people (23.8%)).
From this study we expect that the society would now know about the disease founnd in the prostate gland, particularly BPH. This disease has some symptoms such as being unable to urinate, halting urination or weak emission of urine, painful urination, bleeding urination, and even lower back pain. This disease sometimes also has similar symptoms with other diseases, namely Urinary Tract Stones, in which the patients often complain of halting and bleeding urination. It is expected that BPH patients conduct further investigation to know the development of the disease such as knowing the size of the prostate volume and whether it is malignant or not, in order for them to prevent its recurrence.
The author has not declared any conflict of interests.
REFERENCES
|
Amalia R (2010). Risk Factors in occurrence of Benign Prostate Enlargement (Case Study on RS Kariadi, RSI Sultan Agung, Semarang Roemani RS). Semarang: Diponegoro University School of Medicine.
|
|
|
|
Arif M (2007). Medicine Capita Selecta. 6thEdition. Editor Suprohaita. Jakarta. Media Aescalapius. FK UI: pp. 329-330.
|
|
|
|
|
Association of Indonesia's Urologists (2009). Guidelines for Management of BPH in Indonesia. Available from:
View. [Accessed 9Mei 2016] pp. 1-15.
|
|
|
|
|
Fjellestad-Paulsen A, Höglund P, Lundin S, Paulsen O (1993). Pharmacokinetics of 1-deamino-8-D-arginine vasopressin after various routes of administration in healthy volunteers. Clin. Endocrinol. 38(2):177-182.
Crossref
|
|
|
|
|
Fowler C, McAllister W, Plail R, Karim O, Yang Q (2005). Randomized evaluation of alternative electrosurgical modalities to treat bladder outflow obstruction in men with benign prostatic hyperplasia. Health Technol. Assess 9:3-4, 1-30.
|
|
|
|
|
Glina S, Felipe G (2013). Phatogenic mechanism linking benign prostatic hyperplasia, lower urinary tract symptoms and erectile dysfunction. Therapeutic Advances in Urology. 5(4):211-8.
Crossref
|
|
|
|
|
Gravas S, Bachmann A, Descazeaud A, Drake M, Gratzke C, Madersbacher S, Mamoulakis C, Oelke M, Tikkinen KAO (2015). Guidelines on the management of non-neurogenic male lower urinary tract symptoms (LUTS), incl. Benign Prostatic Obstruction (BPO). European Association of Urolog.
|
|
|
|
|
Hindley RG, Mostafid AH, Brierly RD, Harrison NW, Thomas PJ, Fletcher MS. (2001). The 2-year symptomatic and urodynamic results of a prospective randomized trial of interstitial radiofrequency therapy vs transurethral resection of the prostate. BJU Int. 88:217-220.
Crossref
|
|
|
|
|
January 2012-December 2013. Medan: Faculty of Medicine, University of North Sumatra.
|
|
|
|
|
Kuspriyanti NP (2015). The comparison of genesis urolithiasis based on the Characteristics of patients with benign prostatic hyperplasia. Bandung: Bandung Islamic University School of Medicine.
|
|
|
|
|
Madersbacher S, Schatzl G, Djavan B, Stulnig T, Marberger M (2000). Long-term outcome of transrectal high- intensity focused ultrasound therapy for benign prostatic hyperplasia. Eur. Urol. 37:687-694.
Crossref
|
|
|
|
|
Nickel JC, Mendez CE, Whelan TF, Paterson RF, Razvi H (2010). Update: Guidelines for the management of benign prostatic hyperplasia. Can. Urol. Assoc. J. 4(5):310-316.
Crossref
|
|
|
|
|
Presti JC (2016). Benign Prostatic Hyperplasia incidence and epidemiology www.Health.am. [Accessed May 10, 2016]
|
|
|
|
|
Presti JC, Kane CJ, Shinohara K, Carroll PR (2008). Neoplasms of the Prostate Gland.In: Tanogho, E.A., McAninch, J.W., Smith's General Urology. 17th Ed. USA: Lange, 348:350-351.
|
|
|
|
|
Purnomo BB (2011). Fundamentals of Urology. 3rd Edition. Jakarta: Sagung Seto. 51-55, 57, 75, 124, 127, 129-131.
|
|
|
|
|
Rembratt A, Graugaard-Jensen C, Senderovitz T, Norgaard JP, Djurhuus JC (2004). Pharmacokinetics and pharmacodynamics of desmopressin administered orally versus intravenously at daytime versus night-time in healthy men aged 55-70 years. Eur. J. Clin. Pharmacol. 60(6):397-402.
Crossref
|
|
|
|
|
Roar JK (2015). The Characteristics of Patients with Benign Prostate Hyperplasia (BPH) Undergoing Transurethral Resection of the Prostate (TURP) in the General Hospital Haji Adam Malik in period of Roehrborn CG, Nuckolls JG, Wei JT, Steers W (2007). BPH registry and patient survey steering committee. The benign prostatic hyperplasia registry and patient survey: Study design, methods and patient baseline characteristics. BJU Int. 100:813-819.
|
|
|
|
|
Tanagho E (2008). Smith's General Urology. 17. Issue Editor Jacle W. USA: The McGraw Hill Companies. P 574.
|
|
|
|
|
Vesely S, Knutson T, Damber JE, Dicuio M. Dahlstrand C (2006). TURP and low energy TUMT treatment in men with LUTS suggestive of bladder outlet obstruction elected by means of pressure-flow studies: 8-year follow-up. Neur. Urodyn, 25:770-775.
Crossref
|
|