ABSTRACT
Unwanted pregnancy can occur due to unprotected sexual intercourse and condom breakage. To prevent such problem, emergency contraceptives is the only method that can be used after unprotected sex. This study aimed to assess emergency contraceptive utilization and associated factors among regular undergraduate female students of Wollo University. A cross sectional study was conducted from April 1 to 15, 2017. Simple random sampling was used and 508 study subjects participated with response rate of 100%. Among the total respondents, 41.9% had sexual intercourse at least once prior to this study. Of those who had sexual intercourse, 19.7% had sexual intercourse without condom/contraception. From all respondents, 68.1% of the respondents have ever heard about emergency contraception, but only 30.9% used emergency contraception after unprotected sexual intercourse. Currently, unmarried students were 3.8 times more likely to use emergency contraceptive than currently married students (AOR: 3.8, 95% CI: 0.904 to 0.269). Those students who began sexual intercourse at age 13 years or less were 4.7 times more likely to use emergency contraceptive than those students who began sexual intercourse above age 13 years (AOR: 4.7, 95% CI: 1.403 to 15.769). Emergency contraceptive utilization was low among sexually active students after unprotected sexual debut. Sexual and reproductive health education program should be set up for the university students to avail accurate information about emergency contraception.
Key words: Emergency cotraceptive use, Wollo University, female students.
Emergency contraception refers to a group of birth control modalities that, when used after an unprotected sexual intercourse or contraceptive failure within defined time limits and can prevent an unwanted pregnancy (Kassa et al., 2012; WHO, UNICEF, UNFPA, 2007). Sex during the fertile period without a modern form of contraceptive was most common in the student population. When used properly, emergency contraception can prevent unwanted pregnancy (Wambugu and Njeri, 2013; Manena, 2007). Widespread use of emergency contraception could be a potential strategy to reduce the incidence of unwanted pregnancies and unsafe abortions (Wambugu and Njeri, 2013). Worldwide, annually, over 500,000 women die as a result of childbirth or complication due to unintended pregnancy. Almost all or 99% of these deaths occur in developing countries (Tarekegn et al., 2014). Asia and Africa alone take 95% of the share of the world’s maternal death (Birmeta et al., 2013). World Health Organization (WHO) estimates that 13% of worldwide maternal deaths are due to unsafe abortions secondary to unintended/unwanted pregnancy. Some women with unintended pregnancies obtain abortions and many of which are performed in unsafe conditions and others carry their pregnancies to term, incurring risks of morbidity and mortality higher than those for adult women (Ethiopian Central Statistics Agency and Calverton, 2016).
Ethiopia is one of the top five countries with the highest number of maternal deaths worldwide. The data show a steady decline in the Maternal Mortality Ratio (MMR) for the 7-year period preceding the surveys: from 871 deaths per 100,000 live births in the 2000 Ethiopian demographic and health survey (EDHS), to 673 deaths per 100,000 live births in the 2005 EDHS, and to 676 deaths in the 2011 EDHS, to reach 412 deaths per 100,000 live births in the 2016 EDHS (Nasir, 2010). Despite the availability of highly effective methods of contraception, many pregnancies are unplanned and unwanted. Adolescent pregnancy can lead to serious social stigma, school dropout and decreased school performance and health consequences for both mother and child. The adverse social and economic consequences for an adolescent who becomes pregnant will depend on her particular marital, cultural, familial, and community situation. By preventing unwanted pregnancy, emergency contraceptives can help avert the risks to the mother and child associated with unwanted/unintended pregnancy and childbearing (Habtamu et al., 2014).
The practice of emergency contraception is rare in Ethiopia. As a result of this, the health consequences related to unintended pregnancy and its complications are devastating the lives of adolescents (Kawakatsu et al., 2014). There are few studies which document the extent of emergency contraception use and the influencing factors on its use among university female students in Ethiopia. This study was carried out to determine emergency contraceptive use and its associated factors among undergraduate regular female students of Wollo University to assist policy makers in developing appropriate evidence-based strategies to promote the need based use of emergency contraceptive methods amongst eligible individuals at higher institutions to prevent unintended pregnancy, unsafe abortions, related social stigma, school dropout, maternal morbidity and mortality in Ethiopia.
Study design, population, period and area
A cross sectional study design was deployed among Wollo University undegraduate female students from April 1 to 15, 2017. Wollo University is one of government universities in Ethiopia which is located 401 km from Addis Ababa to the north at Dessie town and was established in 2007. According to the statistics obtained from student service center, currently, the University run 50 undergraduate and 8 post graduate programs in Dessie campuses, and it has a total of 8,585 students with female students accounting for 2,643 (30.8%). The university has one clinic which provides health services to students and there is one government referral hospital in Dessie town which provides service to the population of surrounding areas including Wollo University students. The University has five colleges, two schools and one institute. The source populations for this study were all regular undergraduate female students of wollo University and randomly selected regular undergraduate female students were the study population. Regular undergraduate female students were included and those female students who attend Extension and summer programs in Wollo University were excluded from the study.
Sample size determination and technique
The sample size was calculated using single population proportion formula. By taking into consideration, 18.4% of proportion of emergency contraception practice (Dejene et al., 2009), 95% confidence level, 5% tolerable margin of error, possible non-response rate of 10% and design effect of 2, a total sample of 508 was taken. To check for the adequacy of the sample size, Epi info was used by considering factors associated with emergency contraceptive (EC) use. By comparing sample size based on single population proportion formula and Epi-info, the sample size determined by single population proportion was greater than that of the Epi-info. Therefore the largest sample size of 508 was taken.
After calculating the sample size, all colleges and departments according to their year of study were considered in the sampling process for the selection of the study subjects. Total regular undergraduate female students in Wollo University were stratified into their respective year and colleges, and the sample size was distributed to each department in all colleges using proportional allocation to their size. The study subjects were selected from each department using simple random sampling from active list of each college registrar.
Data collection tools, procedures and quality control
Structured self-administered questionnaire was adapted after review of different literatures in English and translated into Amharic and back translated to English to check its consistency. Ten clinical nurse data collectors’ two health officer supervisors were recruited and underwent one day training on how to organize and orient the study subjects in the arranged room. Pre-test was done on 26 (5%) of sample size at Dessie Health Science College female students and necessary correction was made on the questionnaire based on findings of pre-test before actual data collection. To avoid information exchange, cheating, and bias, all sampled students were gathered in 10 class rooms and sat separately on different seats in Wollo University at the same time, and then structured self-administered questionnaires were distributed after orientation on how to fill the questionnaire.
Finally, the sample students completed filling the questionnaire and returned them to the carton-boxes which were prepared for collection of the filled-questionnaire to minimize social desirably bias. At the end of the data collection, the questionnaires were reviewed and cross checked for completeness by supervisors and the investigator.
Data processing and statistical analysis
Data were entered into Epi-Data 3.02 and exported, cleaned and analyzed by SPSS version 21. The collected data were processed by categorizing the questions, coding computerization and preparation of tables and diagrams; the above procedure helps to minimize data error. Missed data were explored and normality for variables was checked by p-p plot. Descriptive statics for continuous variables, proportion for categorical variables, Odds ratio to check for the strength of association, bivariate and multiple logistic regression analysis were performed. Candidate variables with P-value less than 0.25 in the bivariate analysis was included in the multiple logistic regression analysis using backward stepwise method to develop model and identify predictor factors for emergency contraceptive use. Then, variables P-value of less than 0.05 was taken as significant. The result was organized and presented using tables, graphs, charts and statement.
Ethical consideration
Ethical clearance was obtained from Research Ethics Committee of Wollo University College of Medicine and Health Sciences Department of Public Health. Informed consent from study subjects prior to interview was obtained. The study participants were informed about the purpose of the study and the importance of their participation in the study by contributing information that may help in assessing the practices of female students towards emergency contraceptives. Also the study subjects were informed that they can skip question that they did not want to answer fully or partly and also to stop at any time if they want to do so. Confidentiality of the information was assured by not including their name and ID number and privacy of the respondents was maintained by using self-administered questionnaire.
Operational definition
Emergency contraception (EC):
This is a contraception method that can be used within 72 h following unprotected intercourse to reduce risk of pregnancy.
Unwanted/intended pregnancy
This is a pregnancy that has occurred when the woman does not want to have children, which may be because she already had the desired number of children or it may not be time.
Knowledge
By using index measurement, the graph was skewed to the right, so the data was not distributed symmetrically; the median index was used to classify mothers with good knowledge and poor knowledge.
Attitude
By using index measurement, the graph was distributed symmetrically; so the mean was used to classify mothers with positive attitude and negative attitude.
Women with unmet need for contraception
Women that want to avoid a pregnancy but are not using any method.
Emergency contraceptive use
A study subject who have ever used it to prevent unplanned pregnancy after unprotected sex, or regular contraceptive method failure.
Socio-demography characterstics of participants
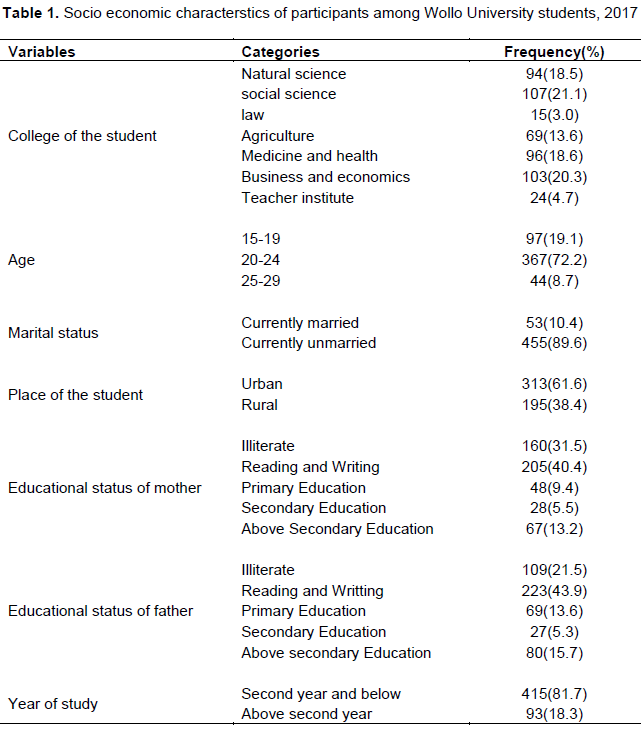
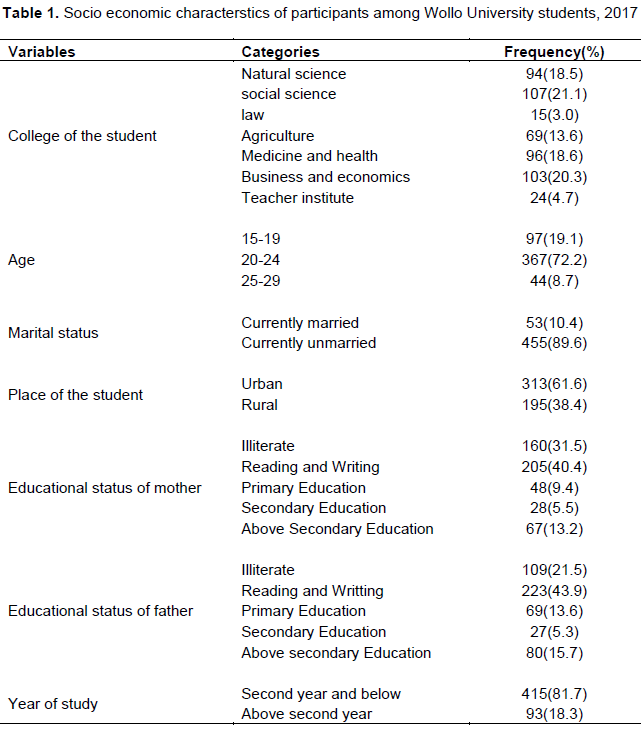
A total of 508 students completed the questionnaire with overall response rates of 100%. The age of the study participants ranged from 18 to 29 years, with mean age of 21.1 years and ± 2.09 SD. Most of the respondents (367, 72.2%), were within the age group of 20 to 24 years. Majority of the respondents (455, 89.6%) were not married currently and 313 (61.6%) were from urban origin (Table 1).
Sexual and reproductive related factors
Among the total respondents who were asked about sexual intercourse, 213 (41.9%) of them had sexual intercourse at least once. The mean and median ages of starting sexual intercourse were 18 years old. Of those who had sexual intercourse, 42 (19.7%) of them had sexual intercourse without condom/contraception. Number of sexual partner in life among regular undergraduate female students showed that 79.5% had 3 and above sexual partner. This indicates risky sexual behavior. Regarding pregnancy of the total sexually experienced respondents, 42 (8.3%) reported ever experiencing pregnancy. Of the participants who experienced pregnancies, 35 (10.6%) and 7 (89.4%) experienced two or less times and three or more times pregnancies, respectively.
From these, 38 (90.5%) of pregnancies were unplanned, and the major reason for these unplanned pregnancies was unavailability of contraception methods which accounts for 19 (50%), followed by condom breakage/slippage and infrequent sexual intercourse without condom which accounts for 18.4 and 15.8%, respectively. Some female respondents reported experiencing abortion due to unwanted pregnancy. From the total number of ever had pregnancy, 33 (86.8%) experienced abortion for a maximum of two times, and 20 (60.6%) and 13 (39.4%) had their abortions in a health facility and traditional place/home, respectively. As respondents noted, the reasons for the abortion were fear of families and not to discontinue their education, which accounts for 17 (51.5%) and 16 (49.5%), respectively.
Knowledge and previous practices of contraception
All the respondents have ever heard about at least one contraception method, 116 (22.8%) have heard about less than four types of contraception methods and 392 (77.2%) have heard about four and more types of contraception methods.
The major source of information about contraception was health professionals (76%) followed by teachers (8.5%). From all respondents, 434 (85.4%) believed on contraceptive methods as they are protective of pregnancy and 346 (68.1%) knew the methods of contraception to prevent unwanted pregnancy after unprotected sexual intercourse. From all respondents, 346 (68.1%) have ever heard about emergency contraception method.
Attitude towards emergency contraceptive
Among all respondents, 158 (31.1%) did not consider the university clinic as convenient for emergency contraceptive usage. For inconveniency of emergency contraceptive usage in the university, 52 (33%) of the respondents’ reason were un-respectful approach of health workers who worked in the university clinic, followed by other reasons (30.4%), inconveniency of time (18.0%), unavailability of drugs (8.2%), lack of privacy (6.3%), and health workers unwilling/unfriendly nature (3.2%). Most of the students have positive attitude towards using emergency contraceptive after unprotected sexual intercourse. Some of the positive attitudes reported by the respondents were: 417 (82.1%) respondent support use of EC after unsafe sex by all female, and 352 (69.3%) of the respondents support availing EC for all females in the university but 91 (17.9%) of the respondents disagreed with recommendation of other female students to use emergency contraception after unprotected sexual intercourse due to religious prohibition (66%), fear of side effects (32.9%), and fear of friends, providers, parents.
Emergency contraceptive utilization
About 449 (88.4%) of the respondents had knowledge of taking emergency contraception after unprotected sexual intercourse but only 157 (30.9%) used emergency contraception after unprotected sexual intercourse to prevent unwanted pregnancy. The commonly used emergency contraceptives were combined oral contraceptive (COC) pills (82.8%) followed by progestogen-only pills (POP) (5.1%) and did not remember (12.1%). Of those who did not use emergency contraception methods (351, 69.1%), 278 (54.7%) was due to fear of side effects, 51 (10.0%) was due to lack of privacy, 16 (3.1 %) was due to lack of knowledge, and 5 (1.0%) was due to fear of parental disapproval. Time of intrauterine contraceptive device (IUCD) insertion among respondents within 72 h was 131 (25.8%), within 5 days was 87 (17.1%), and “I do not know” was 290 (57%). Regarding to the efficiency of EC pills, 46 (57.1%) responded that the efficiency of emergency contraception to prevent unwanted pregnancy was 50%, but 160 (25.8%), 54 (17.1%), and 51 (10%) of the respondents said it was 99, 75, and below 30% efficient in preventing unwanted pregnancy. The remaining 197 (38.8%) of the respondents did not know the efficiency of emergency contraception to prevent unwanted pregnancy.
Bivariate and multivariate analysis of factors associated with emergency contraceptive use
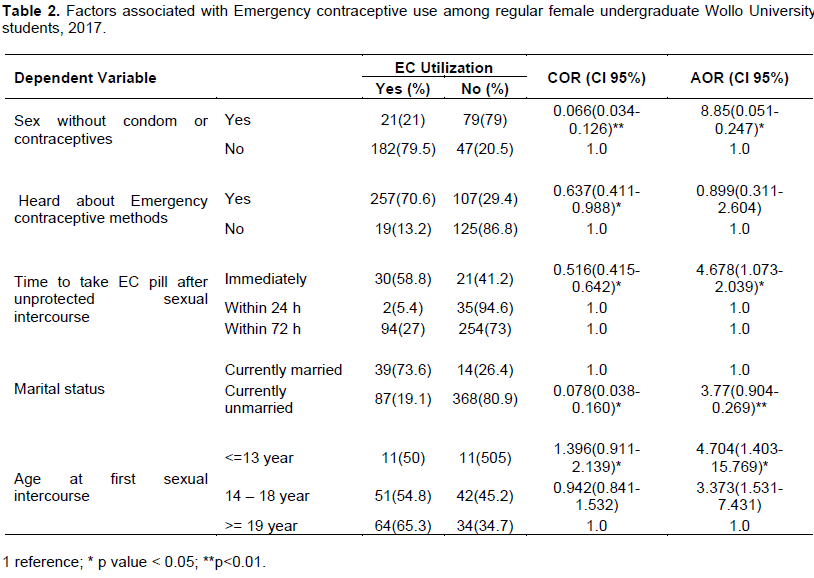
Sex without condom/contraceptives, time to take emergency contraceptive pill after unprotected sexual intercourse, marital status, and age at first sexual intercourse, have significant association with students of EC utilization in multivariate analysis. Currently, unmarried students were 3.8 times more likely to use emergency contraceptive after unprotected sexual intercourse than currently married students (AOR: 3.8, 95% CI: 0.904 to 0.269). Those students who began sexual intercourse at age 13 years or less were 4.7 times more likely to use emergency contraceptive than those students who began sexual intercourse above age 13 years (AOR: 4.7, 95% CI: 1.403 to 15.769) (Table 2).
Although emergency contraception is not recommended as a regular family planning method, it is a useful method after unprotected sexual intercourse to reduce the chance of unwanted pregnancies. Emergency contraception is most useful when there is a failure of barrier methods such as slippage and breakage of condoms, or when sexual intercourse was unplanned (Munro et al., 2012). The overall emergency contraceptive utilization among the study participant was 157 (30.9%), which is greater than the results from the studies conducted in South African (1%) (Manena, 2007), hostels of the University of Nairobi, Kenya (4.4%) (Manena, 2007), Debremarkos University (11.4%) (Habtamu et al., 2014), Jima University (22.2%) (Nasir, 2010), and Addis Ababa University and Unity University College (5%) (Wegene and Fikre, 2007) but lower than the results of the studies conducted in Kampala University, Uganda (45.1%) (Nsubuga, 2016), Jimma University (41.9%) (Nasir, 2010), Princeton University students (8%) (Wambugu and Njeri, 2013) and Adama University (34.8%) (Dejene et al., 2009). The possible reason for such higher prevalence of EC use in this study could be time variation related with currently accelerated RH promotion activities and youth friendly programs in the country and increasing availability of EC in many government and non-government health institutions.
Three hundred and forty eight (68.5%) students had identified the correct timing of administration of the pills after unexpected sexual contact within 72 h, which is higher than the reports from Jimma University (30%) (Nasir, 2010) and Addis Ababa and Unity University college (10%) (Wegene and Fikre, 2007). The possible reason may be linked to the source of information; health personnel/institutions that have good information on the subject than peers/friends and time difference may also be one reason. In addition to this, marital status can also be one reason.
The findings of this study showed that 68.1% of the respondents heard about emergency contraception to prevent unwanted pregnancy after unprotected sexual intercourse which is higher than a study in AAU (43.5%) Wegene and Fikre, 2007; Jimma University (41.9%) (Nasir, 2010) and Harramaya University (25.7%) (Berhanu and Nigatu, 2011). Findings from this study showed that majority of the respondents (46%) started first sexual intercourse at age 19 and above, with the mean and median age of 18.35 and 18, respectively, which is almost similar to the study at Debremarkos University in which 74% of respondents started sex between the ages 15 and 19 years, and the mean age at first sex was 18.7 years (Habtamu et al., 2014) and Haramaya University with mean and median ages of starting sexual intercourse at 18.18 and 18, respectively (Berhanu and Nigatu, 2011). In this study, currently unmarried students were 3.7 times more likely to use emergency contraceptive after unprotected sexual intercourse than currently married students which is lower than a study done at Debremarkos University (Habtamu et al., 2014) in which married respondents were 7 times more likely to utilize EC than those never married respondents, but in a study done at AAU, married students response was compared to not married (Wegene and Fikre, 2007). The possible reason may be that the service sites may not be convenient to married clients. This study showed that students who have sex without condom or contraceptives were 8.85 times more likely to use emergency contraceptive than those who had sex with condom or contraception. Based on this study, students who use emergency contraceptive were 4.678 times more likely to take it immediately after unprotected sexual intercourse than those who took it within 24 h, within 72 h, or within 4 to 6 days.
From this study, risky sexual practices among female students were so high. Knowledge and attitude towards emergency contraceptive among the regular under graduate female students in this University was good. Even if students heard about emergency contraceptive their utilization after unprotected sex was low. Even among those who were aware, utilization and timing of emergency contraceptive was very low. Sex without condom/contraceptives, time to take emergency contraceptives after unprotected sexual intercourse, marital status, and age at first sexual intercourse are determinant factors for utilization of emergency contraceptives.
Limitations
Self-reported information is subjected to reporting biases. Since the study touches sensitive issues the possibility of underestimation cannot be excluded.
Based on the findings and conclusions of the study, the researchers present the following recommendations:
For Wollo University College of Medicine and Health Sciences
(i) More information on human sexuality, conception, and contraception should be made available to female students once they join the university to eliminate misconceptions about contraceptives.
(ii) A similar research has to be undertaken to include male students in the study.
For Wollo University Clinic
(i) Female students should be empowered to take responsibility for the use of contraceptives, by enlightening them with proper and adequate information about their function, usage and methods.
(ii) Girls should have access to confidential counseling and quality contraceptive information and service, including emergency contraception, where appropriate.
For Female Affaire Office
(i) Effort should be put to promote active involvement and participation of male students/partners in the reproductive health services. They could do this through education and participating in campaigns organized by the Department of Health.
(ii) There is a need to educate adolescents about emergency contraceptives, with emphasis on available methods and correct timing of use. There should be promotion of emergency contraceptives to enhance their use and easy accessibility in hospital, pharmacies and student clinic.
The authors have not declared any conflict of interests.
REFERENCES
|
Berhanu D, Nigatu R (2011). Emergency Contraception among Female Students of Harramaya University, Ethiopia: Surveying the Level of Knowledge and Attitude.
|
|
|
|
Birmeta K, Dibaba Y, Wolde YD (2013) Determinants of maternal health care utilization in Holeta town, central Ethiopia. BMC Health Serv. Res. 13(1):256.
Crossref
|
|
|
|
|
Dejene T, Tsion A, Tefera B (2009). Knowledge, Attitude and Practice of Emergency Contraceptives among Adama University Female Students, Ethiopia.
|
|
|
|
|
Ethiopian Central statistics Agency, Calverton M (2016). Ethiopia Demographic and Health Survey report.
|
|
|
|
|
Habtamu A, Muleta M, Dube J (2014). Knowledge, Attitude, Utilization of Emergency Contraceptive and Associated Factors among Female Students of Debre Markos Higher Institutions, Northwest Ethiopia.
|
|
|
|
|
Kassa N, Berhane Y, Worku A (2012). Predictors of unintended pregnancy in Kerssa, eastern Ethiopia. BioMed. Central 9:1.
|
|
|
|
|
Kawakatsu Y, Sugishita T, Oruenjo K, Wakhule S, Kibosia K, Were E (2014). Determinants of health facility utilization for childbirth in rural western Kenya: cross-sectional study. BMC pregnancy childbirth 14(1):265.
Crossref
|
|
|
|
|
Manena N (2007). Knowledge, perception and attitude regarding contraceptives among secondary school learners in the Limpopo province, South Africa.
|
|
|
|
|
Munro ML, Rietz, MF, Seng JS (2012). Comprehensive Care and Pregnancy, the Unmet Care Needs of Pregnant Women with a History of Rape. Informal Healthcare, Issues in Mental health Nursing. 33:882-896.
Crossref
|
|
|
|
|
Nasir T (2010). Knowledge, attitude, and practice of Emergency contraception among graduating female students of Jimma university, south west Ethiopia.
|
|
|
|
|
Nsubuga H, Sekandi N, Hassard S, Fredrick EM (2016). Women's Health Contraceptive use, knowledge, attitude, perceptions and sexual behavior among female University students in Uganda: a cross-sectional survey. BMC Women's Health 16:6
Crossref
|
|
|
|
|
Tarekegn SM, Lieberman LS, Giedraitis V (2014). Determinants of maternal health service utilization in Ethiopia: analysis of the Ethiopian Demographic and Health Survey. BMC pregnancy childbirth 14(1):161.
Crossref
|
|
|
|
|
Wambugu C, Judy N (2013). Factors influencing the use of emergency contraceptive pills among female undergraduate students in main campus hostels of the University of Nairobi, Kenya.
|
|
|
|
|
Wegene T, Fikre E (2007). Knowledge, attitude and practice on Emergency Contraceptives among female students at higher education's in Addis Ababa. Ethiopian J. Health Dev. 21(2):111-116.
|
|
|
|
|
World Health Organization (WHO), United Nations International Children's Emergency Fund (UNICEF), United Nations Fund for Population Activities (UNFPA) (2007). World Bank. Maternal Mortality in Estimates.
|
|