ABSTRACT
In spite of all the various programs and strategies to promote the use of research finding, there is still gap between theory and practice. A number of studies from various countries have reported that nurses’ experience of evidence-based practice is low. In Ethiopia, there is an information gap on the extent of evidence based nursing practice and its associated factors. The study aims to assess the implementation of evidence based nursing practice and associated factors among nurses in Jimma zone public hospitals. Institution based cross-sectional study was conducted from March 1-30/2015. A total of 333 sampled nurses for quantitative and 8 in-depth interview of key informants were involved in the study. Semi-structured questionnaire was adapted from funk’s BARRIER scale and Friedman’s test. Pretest was done on 17 nurses of Bedele hospital. Multivariable linear regression was used to determine factors of evidence based nursing practice. Of 333 distributed questionnaires, 302 were completed, giving 90.6% response rate. Of 302 participants, 245 were involved in EBP activities different levels. About 45 (18.4%) had implemented evidence based practice to low level, 42% had implemented evidence based practice to medium level and 39.6% of the respondents had implemented evidence based practice to high level. The first greatest perceived barrier was setting characteristic. Knowledge about research evidence was positively associated with implementation of evidence based nursing practice. Similarly, place of graduation was positively associated with implementation of evidence based nursing practice. Small number of participants had implemented EPB frequently. Evidence-based nursing practice was positively associated with knowledge of research, place where respondents graduated, and the availability of information resources. Organizational factors were found to be the greatest perceived barrier. Intervention programs on awareness creation, training, resource provision, and curriculum issues to improve implementation of evidence based nursing practice by stakeholders are recommended.
Key words: Evidence based practice, nursing practice, research utilization Ethiopia.
Evidence based practice (EBP) is the use of best research finding (evidence) to answer a burning clinical question together with one’s own clinical expertise generated from outcome management or quality improvement projects and patient preference and values. Researchers generate new knowledge through rigorous research (external evidence) and EBP provides clinicians the tools to translate the evidence into clinical practice and integrate it with internal evidence to improve the quality of health care and patient outcomes (Melnyk and Fineout-Overholt, 2004). Its basic principles are that practical decision made should be based on research studies and that these research studies are selected and interpreted according to some specific norms and characteristic for EBP. EBP utilizes the most up to date methods of providing care, which have been proven through appraisal of high quality studies and statistically significant research finding (Wikipedia, 2014). Health care that is evidence-based and conducted in a caring context leads to better clinical decision and patient outcomes. Gaining knowledge and skill in the EBP process provides nurses and other clinicians the tools needed to take ownership of their practice. There are five sequential steps to the EBP process. Step 1: Asking the clinical questions in the Patient/Population, Intervention/Issue of interest, Comparison, Outcome and Time frame (PICOT) format to get more effective evidence. Step 2: Searching for the best evidence to select. Step 3: Critically appraising the evidence. Step 4: Addressing the sufficiency of the evidence to implement or not to implement, and evaluating the outcome of the evidence implementation (Fineout-overholt et al., 2005). In spite of all the programs and strategies to promote the use of research finding, there is still a gap between theory and practice (Penagiari, 2008). And there are many practices that are being implemented in healthcare that have no or little evidence to support their use (e.g. double-checking of pediatric medication, routine assessment of vital signs every 2 or 4 h in hospitalized patients (Melnyk and Fineout-Overholt, 2004).
Difference in outcomes, health inequalities, and poorly performing health service continue to present a challenge to all nurses. Poorly informed decision-making is one of the main reasons to service can fail to be delivered in an optimal way and can also contribute variation in practice which makes less efficient, ineffective, and inequitable. Half of the world’s death could be prevented with simple cost effective interventions; not enough is known about how to make these more widely available to the people who need them. Changing practice is difficult, wastes time and can have unexpected outcome. However, change can be exciting and motivating. Understanding and planning how to take evidence into practice, to action knowledge, is important. This area because it is so critical, has been the subject of an increasing amount of research itself (International Council of Nurses, 2012). All over the world, there is a growing appreciation of the importance and difficulty of evidence based nursing practice (EBNP). As part of international efforts to facilitate the dissemination of EBNP, research has focused on identifying barriers to utilization of EBNP. Identifying such barriers can help international efforts to develop strategies to overcome these. One of these barriers was found to be lacking the knowledge and skills to evaluate research finding (Eizenberg, 2011). A number of studies from various countries have reported that nurses practice EBP and distinct EBP activities to low extent (Bostrom et al., 2013). Researchers have argued that daily practice in nursing care is influenced more by tradition, intuition, and experiences and less by scientific research. Reviews in literature focus on the difficulty that exists trying to apply research finding into practice. The major barriers to the utilization of research finding were found to be the work organization (setting), the adopter (nurse), and presentation of research findings (Eizenberg, 2011).
Even though evidence based health care has been shown to be an efficient and much needed practice worldwide, developing countries have difficulties in accessibility of existing evidence and medical resources than in developed countries. In Africa, EBP implementation is late as compared to developed world. Incorporating evidence-based health care (EBHC) into the African context means setting priorities, developing evidence summaries, and guidelines and implementing research finding relevant for African countries to support health care for all. Contextualizing evidence relates to several issues, including the lack of evidence available for an African setting. The effectiveness of an intervention in Africa may be different from that found in studies elsewhere because of factors such as: later presentation, co-infections, malnutrition, higher levels of self-medication and use of traditional, reduced level of resources, including human resource for basic health care and political instability. In addition, effective interventions, as determined by many systematic reviews, may not be available or affordable in most African settings. This means that Africa needs valid African-specific research and that authors of systematic reviews should consider this by avoiding overgeneralization when making conclusion (Forland et al., 2013). In Ethiopia, the federal ministry of health lacks skilled health professionals who could help to synthesize evidence for policy-making. Moreover, at all levels of the health systems there is little culture or tradition of trusting or using evidence (Gautham et al., 2014). Also in Ethiopia as well as in the study area there is a gap of shortage of research articles published concerning EBP utilization. This study seeks to explore level of EBP implementation and will give information concerning factors, which hinder implementation of EBP among nurses working in Jimma zone public hospitals.
Study setting and design
Institution based cross-sectional study was conducted from in four public hospitals found in Jimma zone, Oromia Regional State from March 1-30, 2015. Jimma is the town of Jimma zone, which is one of the Oromia Regional States, which is 352 km away from Addis Ababa, the capital city of Ethiopia, in southwestern part of the country.
Study populations
Three hundred and two nurses who were present at work in Jimma Zone public hospitals.
Sample size and sampling procedures
The sample size was determined based on the single population proportion formula and an assumption of 50% was taken, since level of evidence based practice utilization is not known. Assuming a 10% non-response rate, a total sample size of 333 nurses were required. Overall sample was proportionally allocated to each hospital and systematic sampling was used to select participants of the study. All sampled nurses working in four public hospitals of Jimma zone during data collection period were included in the study. Those nurses who were having work experience less than 6 months were excluded.
Data collection
The data was collected using pre-tested semi-structured questionnaire adapted version of Funk’s BARRIERS scale to measure nurse’s perceived barrier of research utilization and Friedman’s test was used to measure knowledge of respondents (Eizenberg, 2011). This questionnaire included the 29-item barrier scale to research utilization. This scale asked the nurses to rate the extent to which they supposed each item as barrier to nurse’s use of research evidence to change or improve their practice. The questionnaire was prepared in English language. The first part of the questionnaire contained items, which measure socio-demographic characteristic of the respondents. The second part of the questionnaire contained questions about awareness and knowledge of evidence based nursing practice. The third part of the questionnaire contained questions about the evidence practice activities. The fourth part of the questionnaire contained questions about source of information and availability of information resources. Part five of the questionnaire contained the ‘BARRIER’ scale, which measured the nurse’s perception on barriers of research evidence utilization. The ‘BARRIER’ scale was divided into four parts (subscales): characteristic of the adopter (nurse’s value, skills, and awareness), characteristic of the organization (setting, barriers and limitation), characteristic of the innovation (qualities of the research) and characteristic of the communication (presentation and accessibility). The subscales Cronbatch’s alpha values were 0.85 for presentation scale, 0.79 for nurse subscale, 0.82 for setting subscale and 0.86 for research (innovation) subscale.
Study variables: Dependent variables implementation of evidence based practice
The scale that measured implementation of EBP in this study includes seven items with minimum score of 7 and maximum score of 35. Moreover, the score on implementation of evidence based nursing practice (EBNP) was transformed into Tertian classification. The higher the score the higher the implementation of EBNP. The independent variables include: socio-demographic factors (age, sex, marital status, qualification, position in the organization and level of hospital), organizational factors (administration support, colleague support, time availability, and incentive for staff), characteristic of individual (communication character, awareness on best evidences, knowledge on research evidence, salary, place of graduation), and characteristic of research evidence (way of presentation, understandability of research report, availability, and accessibility of research reports).
Statistical analysis
The data were carefully entered into Epidata V3.1, edited and cleaned for inconsistencies and missing values. Data was analyzed using SPSS version 16.0. Descriptive statistic was used to summarize data. Bivariate and multivariable linear regression was used to assess the association between dependent variable and independent variables. The variable with p-value less than 0.05 was taken as having significant association.
Ethical considerations
Ethical clearance was obtained from ethical committee of JU (IRB), College of Public Health and Medical Science. A formal letter, from the College of Public Health and Medical Science of Jimma University was obtained and summited to Jimma zone health office and concerned bodies to obtain their cooperation. The purpose of the study was explained to the participants at the time of data collection and written consent was obtained from the participants to confirm whether they will participate or not. The participants of the study were informed that the participation was voluntary based. Confidentiality of the response was ensured throughout the study.
Socioeconomic and demographic characteristics
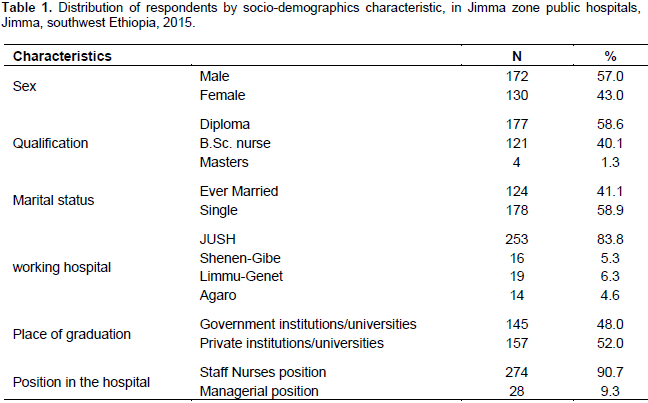
Out of 302 respondents, 57% were male. The mean age was 27 years (SD±6.154), minimum age is 19 and maximum age is 58 years old. Majority were single 178 (58.9%). About 177 (58.6%) of the respondents were diploma holders. About 145 (48.0%) of the respondents were graduate from government higher institution and the rest were graduated from private institutions. About 274 (90.7) were in staff nurses and the rest 28 (9.3%) were in different managerial position (Table 1).
Awareness and knowledge about evidence-based practice
When the respondents were asked how familiar they were with concept, about 190 (62.9%) were familiar with the concept of EBP. When the respondents asked knowledge questions concerning research concept and research terms about 82 (27.2%) of respondents scored low level, about 78 (25.8%) of respondents scored medium level and about 92 (30.5%) of respondents scored high level (based on Tertian classification).
Source of information and availability of the information resource
Concerning the source of information and availability of the information resource, when asked how they evaluate the availability of information resource in the hospital, only 85 (28.1%) said that online resource were available and 76 (25.2%) said that print material were available. Major source of information that respondents usually find evidence for their nursing care practice was internet 118 (39.1%). When asked how often they look for information from the given sources, about 135 (44.6%) were using reference book, about 40 (13.2%) were using research report, about 36 (11.9%) were using journal article and about 41 (13.5%) were using hospital library on the regular bases.
Level evidence based practice activity
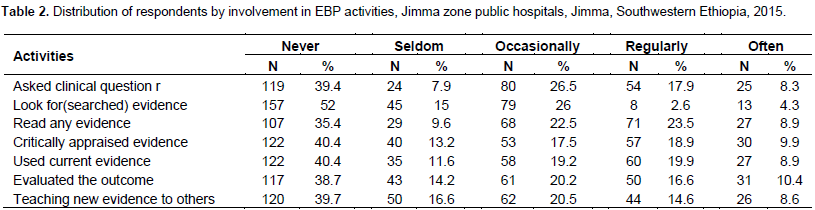
From the total 302 participants, 245 (81.1%) had involved in different EBP activities to different level (from seldom to often). Total score was computed for individuals total score in EBP and Tertian classification was done on the total score of EBP activity measurements. Accordingly, about 45 (18.4%) of the respondents implemented EBP to low level (sometimes), about 103 (42%) of the respondents implemented EBP to medium level and about 97 (39.6%) of respondents implemented EBP to high level (Table 2).
Perceived barriers to research utilization
The top 5 perceived barriers reported in this study were (1) ‘physician doesn’t not cooperate with implementation of new evidences’; (2) ‘the nurse is isolated from knowledgeable colleagues with whom to discuss new findings’; (3) ‘there is no incentive for clinical practice development’; (4) ‘the nurse feels the benefit of changing practice is minimal’; and (5) there is resistance to make change in the work setting. Since 60% of this perceived barrier is from setting origin, the largest perceived barrier was organizational factors (mean =26.60, ±7.08).
Factors associated with implementation of evidence based nursing practice
Factors associated with implementation of EBNP were assessed and the significant association was found between knowledge about EBP and implementation of EBP. Knowledge about EBP was positively associated with EBNP implementation (β=0.76, P=0.008). For a unit increase in knowledge about research, implementation of EBNP increases by 0.762. Similarly, place where the respondent graduated was positively associated with evidence based practice (β=2.270, P=0.047). Graduating from public universities increases evidence based practice by 2.270. Another positively associated variable is extent of resources availability such as internet services (online resource), print materials and other information resources (such knowledgeable colleagues) (β =0.67, P= 0.006). Availability of information resource such internet access increases the utilization of EBP by 0.67 (Table 3).
Participants in this study were involved in each activity of EBP with different levels of involvement, but for simplicity the score was summed up and transformed into Tertian classification. Accordingly, about 45 (18.4%) of the respondents had implemented EBP to low level (sometimes), about 103 (34.1%) of the respondents had implemented EBP to medium level (usually) and 97 (32.1%) of the respondents implemented EBP to high level (always). This finding was consistent with the study done in Sweden by Bostrom et al, 2013 in which (60%), approximately similar level of EBP implementation was reported (19% asked clinical questions and performed searches in data bases, 56% used information sources, 31% appraised the literature, 30% participated in practice development, and 34% participated in evaluating clinical practice to high extent) (9, 13). Also finding from this study was analogous with the study conducted in South Africa, in which 35.6, 32.9, and 31.5% use EBP frequently, moderately and rarely, respectively. Even though in this study small numbers of respondents were frequently involved in EBP about (18.4 %), the finding is similar with finding from South Africa. On the other hand the finding from this study is higher than the study done in Tikur Anbesa hospital in Addis Ababa, in which 57.6% participants applied EBP. Of them, 64 (52.8%), 38 (31.4%) and 19 (15.7%) applied EBP sometime, usually and always respectively (Hadgu et al., 2015). This could be due the sample size difference. In this study, the sample is somewhat higher than the study done in Tikur Anbesa hospital. The other possible justification may be in Jimma University specialized hospital; there is nursing care standardization program that may increase nurses’ application of new research evidence in their nursing care practice.
Concerning perceived barriers to research utilization from the top 5 reported barriers, 3 were setting related barriers, that is, about 60% were from organizational factors. Therefore, the greatest perceived factor was organizational factors (mean=26.60, SD±7.08). This finding was similar with studies done in USA, China, Iran, Maldives, German, and Australia. In addition, organizational factor has been consistently reported as greatest perceived factor. On the other hand, when we compare top 5 perceived barriers to research utilization with seven other studies except this study, most of the studies reported that ‘insufficient time to read and implement new idea’ was the most reported barrier (Eizenberg, 2011; Uysal et al., 2010; Heydari et al., 2014; Umarani, 2014; Dalheim et al., 2012; Gravel et al., 2006; Retsas, 2000; Schoonover, 2006; Shifaza et al., 2014). In this study, knowledge about EBP was positively associated with EBP implementation (β=0.76, P=0.008). This finding was similar in pattern with study done in USA where nurses who reported having greater knowledge of EBP also reported a greater extent of evidence-based care (r=0.42, p <0.0001) (Melnyk et al., 2004). Similarly, the study done in Iran is in line with this finding where nurses who knew the definition of evidence-based nursing were more likely to utilize research findings in clinical practice than those who did not know (Pearson c2 = 23.912, P = 0.02) (Heydari et al., 2014). Similarly, in our country, one study that was conducted in Tikur Anbesa hospital reported that those nurses who have knowledge were 3 times more likely to practice EBP than those who do not have knowledge (Hadgu et al., 2015).
IMPLICATION FOR PRACTICE, POLICY AND NURSING PROGRAMS
In this study, small number of nurses applied EBP to high level (frequent basis). This means most of the nurse in Jimma zone public hospital uses traditional way of practice, that means depend on the expert opinion and school training, which may be out to date way of practice, which delays the latest way of patient care approach, which enhances the progress of patient outcomes. Since the use of evidence-based practice delivers the positive patient care outcomes nurse in Jimma zone public hospitals should implement EBP in their nursing care practice to positive patient care outcomes. It is very much important to consider nursing care policy and nursing curriculum issues so that curriculum planners should strictly emphasize on EBP philosophy during program preparation. Nursing care policy should empower nurse so that nurses autonomously implement EBP during nursing care practice. Other area that should be considered is educational preparation for nurse particularly in private institutions or colleges. Private nursing college should comply all the issue incorporated in Ethiopia nursing education programs so that graduate from private institution be competent in implementation of research findings in the nursing care practice.
Since this study was based on self-report, the response on the EBP practice may be inflated due to social desirability bias of respondents.
CONCLUSION AND RECOMMENDATIONS
This study concluded that small number of nurses applied EBP to high level. Organizational factors were found to be the greatest perceived barrier. The implementation of evidence-based practice was associated with knowledge on research, place of graduation, and the availability of information resources. The level of perception and level of EBP implementation was not associated. There has to be intervention program to facilitate the implementation of evidence in nursing practice by the respective stakeholders (Ethiopian Federal Ministry of Health, Oromia Regional Health Bureau, educators of nursing education and hospital administration of Jimma zone public hospitals). Training should be conducted for nurses on implementation of evidence-based practice by Jimma zone public hospitals in collaboration with NGOS, Ethiopian Federal Ministry of Health and Oromia Regional Health Bureau. Resources necessary to implement evidence based nursing practice should be provide by hospital administration of Jimma zone public hospitals in collaboration with Ethiopian Federal Ministry of Health, Oromia Regional Health Bureau and other NGOs Intervention programs concerning organizational communication with issue on evidence based practice implementation should be done together with nurses and physician to create supportive staff by hospital administration of Jimma zone public hospitals. Since there is gap of awareness on evidence based nursing practice curriculum planners should take into consideration to include the principle of evidence based nursing practice in Ethiopian nursing education programs especially in the undergraduate nursing education curriculum. Private nursing colleges should incorporate principles of evidence based practice in their nursing education programs so that graduates from private nursing college should be competent.
The authors have not declared any conflict of interests.
The authors would like to thank the respondents who participated in the study. They are also grateful to Jimma University for funding the study.
REFERENCES
|
Bostrom AM, Rudman A, Ehrenberg A, Gustavsson JP, Wallin L (2013). Factors associated with evidence-based practice among registered nurses in Sweden: a national cross-sectional study. BMC Health Services Research, 13(1):165.
Crossref
|
|
|
|
Dalheim A, Harthug S, Nilsen RM, Nortvedt MW (2012). Factors influencing the development of evidence-based practice among nurses: a self-report survey. BMC Health Services Research, 12(1):367.
Crossref
|
|
|
|
|
Eizenberg MM (2011). Implementation of evidenceâ€based nursing practice: nurses' personal and professional factors?. Journal of Advanced Nursing, 67(1):33-42.
Crossref
|
|
|
|
|
Fineout-Overholt E, Melnyk BM, Schultz A (2005). Transforming health care from the inside out: advancing evidence-based practice in the 21st century. Journal of Professional Nursing, 21(6):335-344.
Crossref
|
|
|
|
|
Forland F, Rohwer AC, Klatser P, Boer K, Mayanja-Kizza H (2013). Strengthening evidence-based healthcare in Africa. BMJ Evidence-based Medicine, 18(6):204-206.
Crossref
|
|
|
|
|
Gautham M, Berhanu D, Umar N, Ghosh A, Elias N, Spicer N, Becker A, Schellenberg J (2014). Panel discussion: The challenges of translating evidence into policy and practice for maternal and newborn health in Ethiopia, Nigeria and India. BMC Health Services Research, 4(2):7.
Crossref
|
|
|
|
|
Gravel K, Légaré F, Graham ID (2006). Barriers and facilitators to implementing shared decision-making in clinical practice: a systematic review of health professionals' perceptions. Implementation Science, 1(1):16.
Crossref
|
|
|
|
|
Hadgu G, Almaz S, Tsehay S (2015). Assessment of Nurses 'Perceptions and Barriers on Evidence Based Practice in Tikur Anbessa Specialized Hospital Addis Ababa Ethiopia, 4(3):73-83.
|
|
|
|
|
Hadgu G, Almez S, Tsehay S (2015). Assessment of nurses' perceptions and barriers on evidence based Practice in Tikur Anbessa Specialized Hospital Addis Ababa Ethiopia. American Journal of Nursing Science, 4(3):73-83.
Crossref
|
|
|
|
|
Heydari A, Zeydi AE (2014). Barriers to and Facilitators of Research Utilization among Iranian Nurses: a Literature Review. Journal of Caring Sciences, 3(4):265-275.
|
|
|
|
|
International Council of Nurses (ICN) (2012). Closing the gap from evidence to action 2012. Available at:
View
|
|
|
|
|
Melnyk BM, Fineout-Overholt E (2011). Evidence-based practice in nursing & healthcare: A guide to best practice. Lippincott Williams & Wilkins.
|
|
|
|
|
Melnyk BM, Fineoutâ€Overholt E, Fischbeck Feinstein N, Li H, Small L, Wilcox L, Kraus R (2004). Nurses' perceived knowledge, beliefs, skills, and needs regarding evidenceâ€based practice: Implications for accelerating the paradigm shift. Worldviews on Evidenceâ€Based Nursing, 1(3):185-193.
Crossref
|
|
|
|
|
Panagiari D (2008). Barriers and Facilitators for implementing evidence-based practice among German nurses working in a general hospital (Master's thesis, University of Twente). Available at:
View
|
|
|
|
|
Retsas A (2000). Barriers to using research evidence in nursing practice. Journal of Advanced Nursing, 31(3):599-606.
Crossref
|
|
|
|
|
Schoonover HD (2006). Barriers to research utilization among registered nurses working in a community hospital. Available at:
View
|
|
|
|
|
Shifaza F, Evans D, Bradley H (2014). Nurses' perceptions of barriers and facilitators to implement EBP in the Maldives. Advances in Nursing, 1-7.
Crossref
|
|
|
|
|
Umarani J (2014). Perceived barriers to Evidence Based Practice among Registered Nurses. Asian Journal of Biomedical and Pharmaceutical Sciences, 4(32):15-19.
Crossref
|
|
|
|
|
Uysal A, Temel AB, Ardahan M, Ozkahraman S (2010). Barriers to research utilisation among nurses in Turkey. Journal of Clinical Nursing, 19(23â€24):3443-3452.
Crossref
|
|
|
|
|
Wikipedia (2014). Evidence-based practice. Available at:
View
|
|