ABSTRACT
Proper child positioning and attachment initiates the production of optimal amounts of breast milk and contribute to the comfort of a child during suckling. Poor breastfeeding practices like early cessation and poor breastfeeding skills, introduction of unclean artificial feeding have been widely documented in the world. This cross-sectional community based study was carried out between October 7 and 25, 2013 in Arba Minch Zuria. Structured questionnaires and observational-checklist were used to collect data. The missing values and outliers, data, were checked and entered in double. Multivariable logistic regression was done to identify the predictors of poor and good positioning and attachment to breast. More than one-fifth of 384 (20.1%) infants was poorly positioned and attached to breast. Poor attachment of children to the breast were negatively associated with infant’s age below 6 (AOR=0.03 (0.01, 0.11)), attending breast feeding education (AOR=0.42(0.19, 0.93)) and positively associated with having an uneducated husband (AOR=0.07(0.01, 0.51)). Poor child positioning were also negatively associated with infant’s age below 6 (AOR=0.03(0.01, 0.10)), lack of information on breastfeeding (AOR=0.42(0.19, 0.94)), and early introduction of additional food (AOR=0.44(0.20, 0.97). Overall, in more than one-fifth of mothers (20.1%), the breastfeeding attachment and positioning were found to be lower than the national and global recommendations. It is highly related to infant’s age, paternal educational and an exposure to breastfeeding education. Thus, continuous community based nutritional health education were needed to promote optimal breastfeeding skills using health workers, religious leader and local community resource people as key actors.
Key words: Positioning, attachment, breastfeeding, Arba Minch.
There is a universal consensus on the dietary benefit of optimal breastfeeding practices for children’s optimal growth and mental health benefits. Currently, breastfeeding is the focus of multi-professional interest because of its nutritional value and psychological benefits for both mother and her child. Breastfeeding benefits are short-term and long-term protection of children against malnutrition and infectious disease (WHO, 2002, 2003).
Effective breastfeeding is achieved when the mother and baby are properly positioned and child is attached to the mother's breast. Breastfeeding is an art that could be learned. It has been documented that very few women breastfeed without difficulty from the first day, but majority encounter problems somewhere along the way (FMOH, 2004; WHO and UNICEF, 2008). These difficulties are due to limited feeding time, lack of sureness or poor attachment of the baby at the breast. Study showed an unsettled, hungry and angry baby, breast engorgement, and maybe obstructed milk ducts and reduced milk production are the most common cause of ineffective breastfeeding (FMOH, 2004; WHO and UNICEF, 2008; Belachew, 2003). Mothers and babies should be comfortable during breastfeeding. Proper child positioning and attachment initiate the production of adequate amounts of breast milk and give comfort to a child during sucking and it helps in preventing sore nipples, engorgement and mastitis. For good attachment and successful breastfeeding, it is important to properly position the baby’s body (ThaKre et al., 2012; Goyal et al., 2011; CSA, 2012; FMOH, 2005).
Right positioning and attachment of the baby at the breast are critical in establishing and effective breastfeeding. Early initiation of breastfeeding, skin to skin contact between mothers and babies, breastfeeding on demand, and help with positioning and attaching the baby increase the opportunity of successful breastfeeding. Successful breastfeeding is a result of the appropriate positioning and attachment of the child to the breast (ThaKre et al., 2012; Goyal et al., 2011; CSA, 2012; FMOH, 2005, 2008; Kimani-Murage et al., 2011).
Poor breastfeeding practices have been well documented both in emerging and developed countries. Suboptimal breastfeeding practices like discarding colostrum, overdue initiation of breastfeeding, introduction of dirty and unreliable artificial feeding and poor breastfeeding skills are common constraints to tackling an infant and child mortality in developing countries like Ethiopia (CSA, 2012; FMOH, 2005, 2008; Kimani-Murage et al., 2011).
The baby’s head, neck and trunk should be positioned in neutral alignment to optimize breastfeeding performance. Otherwise it compromises an infant’s ability to feed effectively, as it disturbs respiratory mechanisms, oral motor control and swallowing. If the baby is not properly attached to the breast, it might cause nipple pain and even damage. Limited feeding can result in engorgement of breast, which in turn can lead to poor attachment (WHO, 2002; FMOH, 2008; Kimani-Murage et al., 2011; WHO and UNICEF, 2009; Heck et al., 2006). Although, many scholars recommend that a proper positioning and attachment technique reduces breastfeeding related problems and increases long-term breastfeeding, no studies have been done in the area of Arba Minch Zuria.
Study setting and sample
A cross-sectional community based study was conducted from October 7 to 25, 2013 in Arba Minch Zuria in GamoGofa zone, in the southern part of Ethiopia. The district has an estimated total population of 165,680 of which 82,751 were males and 82,929 were females as it was shown by 2007 published Central Statistical Agency (2008). Nine administrative units (kebeles) were randomly selected from 31 kebeles of the district.
A total of 384 breastfeeding women were included in the study through a single population proportion formula. Since there has been no study done in this area, an estimated 50% prevalence of proper breastfeeding skill and practice was considered with a 5% margin of error, 95% confidence interval. The study included mothers who had children in the last two years and were permanent resident of selected kebeles. Breastfeeding women were randomly selected using a simple random sampling technique.
Data collection procedure
Structured questionnaires and observational-checklist were used to collect socio-demographics characteristics, child feeding practices and environmental health characteristics. Moreover, women’s knowledge on breast milk and breastfeeding skills was also included in the questions. Questionnaires were prepared in English and translated to Amharic, then retranslated back to English by language experts who can speak both languages to check its reliability. The questionnaires were pre-tested for simplicity and clarity. Based on pre-test, additional adjustment was made in terminologies and formatting questionnaires.
Statistical analysis
The data were checked for missing values and outliers and entered in double and analysed using SPSS version 16.0. Descriptive statistics like frequencies and proportion were used to describe the study population in relation to relevant variables. Bivariate associations between predictors and breastfeeding skills were described to see the strength of association using odds ratios and 95% of confidence intervals. Then, to identify the predictors of positioning and attachment grade, only variables that were significantly associated with bivariate analyses were entered into the multivariable logistic regression model with good positioning and attachment as a dependent variable. Multicollinearity among independent variables was checked and no multicollinearity was detected (Egata et al., 2013). All tests were two-sided and P<0.05 was considered as statistically significant.
The observation was evaluated in accordance with criteria set by national breastfeeding recommendations. If infant body and head is straight; head and body is facing breast and well supported with skin-to-skin contact and if the infant’s whole body is supported and all of these four signs are present, breastfeeding skills were graded as well positioned. Missing one or two criteria was graded as average and achieving one criteria or missing all was considered as poor positioning. A child is well attached, if the chin touches the breast and lip is opened widely; lower lip turned downward and areola is more visible above than below. If one of the criteria was not fulfilled, it was considered as an average attachment and achieving one criteria or missing all was considered as poor attachment.
Ethical considerations
Ethical clearance and official permission was obtained from an ethical clearance committee of Arba Minch University and Arba Minch Zuria Woreda administration before the study commenced. And an informed verbal consent was obtained from each study participant for their willingness of participation.
From 384 breastfeeding women, 98.2% gave complete response. The mean (±SD) age of the mothers was 25.08 years (±6.65) with the range of 15 to 40 years. More than one-fourth of infants were well positioned and attached to breast. Inversely, more than one fifth of mothers poorly positioned and attached their infants to breast (Table 1).
The promotion of optimal breastfeeding has been recognized as a global public health concern. Effective breastfeeding is crucial in getting all the benefits of breastfeeding. Breastfeeding has a unique combination of nutritional and immunological benefits for infants and their mothers. Only 28.5% of women appropriately attached their children to breast during breastfeeding, which was relatively low as compared to the study done in Arjo, were 35.97% mothers well attached their children to breast (Tamiru et al., 2012). Similarly, small number of women (28.8%) appropriately positioned their children during breastfeeding which is less than the findings from Jimma Arjo were 33.79% of women appropriately positioned their children during breastfeeding (Rea et al., 1999). As compared to the study done in india, child positioning and attachment during breastfeeding were also relatively low which might be due to lack of knowledge on optimal child feeding practices (ThaKre et al., 2012).
Breastfeeding skills were significantly associated with infant’s age, breastfeeding education and paternal educational levels. Women who had infants aged less than 6 months were more appropriately attached and positioned their infants during breastfeeding as compared to those who had one year and above. This might be due to the size of a child, easy to hold and poor breastfeeding skills. This study also showed that an exposure to breastfeeding education had a significant input for proper child attachment to breast. Women who had information on breastfeeding practised relatively less child attachment to breast. This might be due breastfeeding education given along with other health issues for women. Studies from india and other countries also showed that pre-education is a determinant factor of appropriate child feeding practices (WHO, 2002, 2003; Tamiru et al., 2012).
Paternal education level was significantly associated with good attachment of child to breast. This might be due to the influences of husband involvement and psychological support to optimal breastfeeding practices. Fathers with more education are better informed and aware of the benefits of breastfeeding and encourage their wife on optimal breastfeeding. Women need full support of their families and government to feed their children and family appropriately. Studies also found the positive trends of optimal child feeding improvement with paternal education status (Tamiru et al., 2012; Rea et al., 1999; Tamiru et al., 2012; Law et al., 2007; Kristiansen et al., 2010).
Women who attended breastfeeding education and poorly positioned their children to breast were less than those that did not attend, this could be due to health extension support. This shows that basic education in the promotion of optimal breast-feeding should be heartened. Studies also showed health education given at different juncture regarding breastfeeding practices is the predetermining factors to promote optimal breastfeeding practices (WHO, 2002, 2003; Rea et al., 1999).
Women who introduced complementary food early and poorly positioned their children to breast were 56% more than those that did not introduce complementary food early. This might be due to complementing of breastfeeding with food and maternal gap of knowledge on the breastfeeding skills. Studies from Arjo and national report also demonstrated that maternal knowledge and their educational status has significant input on optimal
child feeding practices (FMOH, 2005; Rea et al., 1999).
Women who had infants below 6 months and 6 to 12 months were 99.92 (AOR=0.03(0.01, 0.11)) and 99.77% (AOR=0.08(0.02, 0.27)) that poorly attached their infants to breast than who had one year and above, respectively. Women who had infants below 6 months were 8 times more well attached (AOR=8.54(8.44, 84.39) than those that had 12 months and above infants (Table 2).
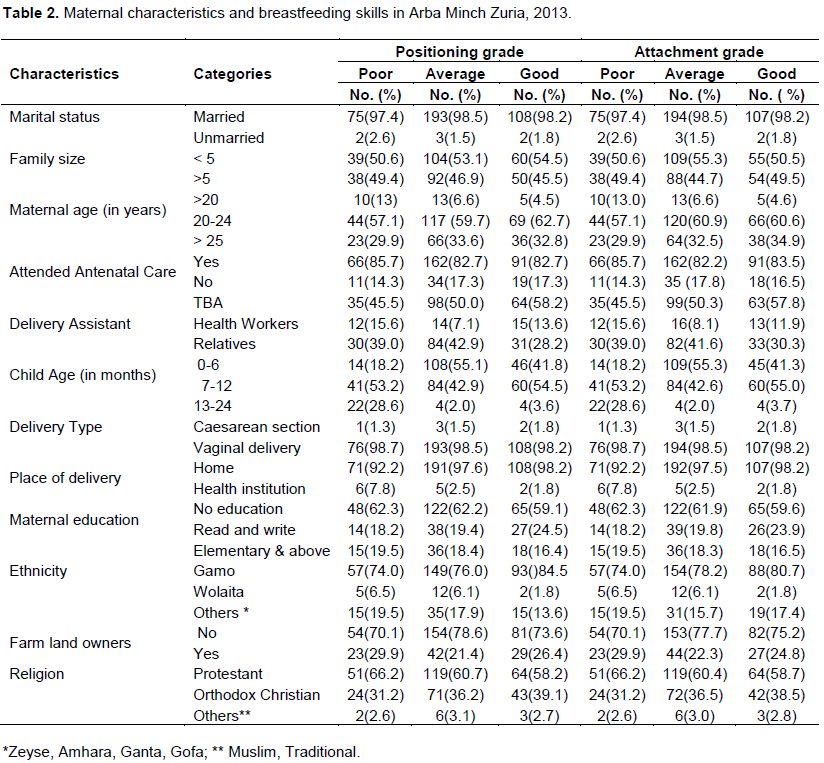
Women who have been informed about the dietary importance of breastfeeding and poorly attached their children to breast were 58% less (AOR=0.42(0.19, 0.93)) than who had no information. Similarly, women who had uneducated husband and poorly attached their children to breast were 99.93% (AOR=0.07(0.01, 0.51)) more than those that had educated husband (Table 3). Similar to breastfeeding attachment, women who had infants below 6 and 6-12 months were 14% times (AOR=8.14(3.04, 1.87)) more well positioned and 99.02% (AOR=0.08(0.02, 0.26)) less poorly positioned than those that had 12 months and above. Women who had information on breastfeeding and attached their children (AOR=0.42(0.19, 0.94)) poorly to breast were 58% less than those that had no information. Women who gave additional food before 6 months and poorly positioned (AOR=0.44(0.20, 0.97) their children to breast were 56% more than those that did not give additional food (Table 4).
More than one-fifth of women poorly positioned and attached their children to breast as compared to national and international recommendations. Poor breastfeeding skills were significantly associated with infant’s age, pre-education on the benefits of breastfeeding and educational status of husband. Hence, sustained community based nutritional education were recommended for pregnant and lactating mothers to encourage optimal breastfeeding skills during the period of attending health care and community meeting through education on breastfeeding using health extension workers, religious personel and development army as key actors.
The authors have not declared any conflict of interest.
REFERENCES
|
Belachew T (2003). Human Nutrition for Health Science Students Jimma, 2003. Published by: Jimma University, Faculty of Public Health.
|
|
|
|
Central Statistical Agency (CSA) (2008). Summary of statistical report of 2007; Population and housing census. Addis Ababa: CSA; 2008.
|
|
|
|
|
Central Statistical Authority (CSA) (2012). Ethiopia Demographic and HealthSurvey 2011. Addis Ababa and Calverton: CSA; 2012 Available at:
View
|
|
|
|
|
Egata G, Berhane Y, Worku A (2013). Predictors of non-exclusive breastfeeding at 6 months among rural mothers in east Ethiopia: A community-based analytical cross-sectional study. Int. Breastfeed. J. 8:8.
Crossref
|
|
|
|
|
Federal Ministry of Health (FMOH) (2005). National strategy for child survival in Ethiopia. Addis Ababa: FMOH; 2005. Available at:
View
|
|
|
|
|
Federal Ministry of Health (FMOH) (2008). Program Implementation Manual of National Nutrition Program. Addis Ababa: FMOH; 2008.
|
|
|
|
|
Federal Ministry of Health: National strategy for infant and young child feeding. Addis Ababa: (FMOH) (2004).
|
|
|
|
|
Goyal RC, Banginwar AS, Ziyo F, Toweir AA (2011). Breastfeeding practices: Positioning, attachment (latch-on) and effective suckling-A hospital-based study in Libya. J. Fam. Commun. Med. 18(2):74.
Crossref
|
|
|
|
|
Heck K, Braveman P, Cubbin C, Chavez, G, Kiely J (2006). Socioeconomic Status and Breastfeeding Initiation among California Mothers. Public Health Rep. 121(1):51-59.
Crossref
|
|
|
|
|
Kimani-Murage E, Madise N, Fotso J, Kyobutungi C, Mutua M, Gitau T, Yatich N (2011). Patterns and determinants of breastfeeding and complementary feeding practices in urban informal settlements, Nairobi Kenya. BMC Public Health 11:396.
Crossref
|
|
|
|
|
Kristiansen AL, Lande B, Øverby NC, Andersen LF (2010). Factors associated with exclusive breast-feeding and breast-feeding in Norway. Public Health Nutr. 13(12):2087-2096.
Crossref
|
|
|
|
|
Law SM, Dunn OM, Wallace LM, Inch SA (2007). Breastfeeding Best Start study: training midwives in a 'hands off'positioning and attachment intervention. Maternal Child Nutr. 3(3):194-205.
Crossref
|
|
|
|
|
Rea MF, Venancio SI, Martines JC, Savage F (1999). Counselling on breastfeeding: assessing knowledge and skills. Bull. World Health Organ. 77:492-498.
|
|
|
|
|
Tamiru D, Belachew T, Loha E, Mohammed S (2012). Sub-optimal breastfeeding of infants during the first six months and associated factors in rural communities of Jimma Arjo Woreda, Southwest Ethiopia. BMC Public Health 12(1):363.
Crossref
|
|
|
|
|
Thakre SB, Thakre SS, Ughade SM, Golawar S, Thakre AD, Kale P (2012). The breastfeeding practices: the positioning and attachment initiative among the mothers of rural Nagpur. J. Clin. Diagn. Res. 6(7):1215-1218.
|
|
|
|
|
WHO and UNICEF (2008). Strengthening action to improve the feeding of infants and young children 6-23 months of age in nutrition and child health programmes. Geneva: WHO; 2OO8.
|
|
|
|
|
WHO and UNICEF (2009). Breastfeeding promotion and support in a baby-friendly hospital. Geneva: WHO; 2OO9.
|
|
|
|
|
World Health Organization (WHO) (2002). The optimal duration of exclusive breastfeeding: A systematic review. Geneva: WHO; 2002.
|
|
|
|
|
World Health Organization (WHO) (2003). Global Strategy for Infant and Young Child Feeding. A joint WHO/UNICEF statement. Geneva: WHO; 2003.
|
|