ABSTRACT
Modern drug therapy of epilepsy is complicated by the inability of drugs to control seizures in some patients and side effects that range in severity from minimal impairment of the central nervous system to death from aplastic anemia or hepatic failure. Medicinal plants used in traditional medicine for the treatment of epilepsy have been scientifically shown to possess promising anticonvulsant activities in animal models for screening for anticonvulsant activity and can be a source of newer anticonvulsants. The aim of this study was to investigate the preliminary phytochemical properties, anticonvulsant and anxiolytic activities of Melanthera scandens aqueous and ethanolic extracts.. Phytochemicals from the aqueous and ethanolic extracts were screened by standard methods. Anticonvulsant activity was evaluated against pentylenetetrazol (PTZ)-induced seizure model in rats. The effect of the extract at oral dose levels of 250, 500 and 1000 mg/kg was evaluated in an experimental rat model, using diazepam (5 mg/kg) as positive control. Anxiolytic activity was performed using elevated plus maze method. Phytochemical screening revealed that M. scandens extracts contain carbohydrates, flavonoids, saponins, glycosides, tannins, terpenoids, phenols and phytosterols. The aqueous extract at a dose of 500 mg/kg significantly increased seizure latency (P=0.0023), while the ethanolic extract did not have a significant effect on seizure latency. Both extracts significantly reduced the seizure severity (P= 0.0155), and provided up to 100% protection against PTZ induced death at 1000 mg/kg. Both extracts had no significant effect on the duration of PTZ induced seizures. Both extracts were found to increase the number of entries and the time spent in the open arms of the maze at a dose of 250 mg/kg, indicating anxiolytic activity, which was not seen at higher doses (500 and 1000 mg/kg). The total numbers of entries into the closed arm were significantly reduced at 500 and 1000 mg/kg oral doses of both extracts, indicating a reduction in locomotor activity of the rats. The results obtained in this study suggest that both the aqueous and ethanolic extracts of M. scandens possess anticonvulsant and anxiolytic activities in a rat model.
Key words: Melanthera scandens, Pentylenetetrazole (PTZ), anticonvulsant, anxiolytic.
Epilepsy is one of the most common and widespread neurological disorders in the human population (Surajit et al., 2012).In modern medicine, epilepsy is considered to be a chronic brain syndrome of various etiology characterized by recurrent seizures and usually associated with loss or disturbance of consciousness.
There may be a characteristic body contraction (convulsion). The seizure is due to excessive electrical discharge in the brain and the seizure pattern depends not only on the cause but the origin, extent, intensity and type of epileptic discharge in the brain (Muazu and Kaita, 2008). Epilepsy is usually controlled, but not cured, with medication (Sridharamurthy et al., 2013). Currently available anticonvulsant drugs are able to efficiently control epileptic seizures in about 50% of the patients; another 25% may show improvement whereas the remainder does not benefit significantly. Furthermore, undesirable side effects of the drugs used clinically often render treatment difficult so that a demand for new types of anticonvulsants exists (Kamalraj, 2011). Anxiety affects most of the population nearly one- eighth of the total population worldwide. About 500 million people suffer from neurotic, stress related and somatoform problems and 200 million suffer from mood disorders.
Benzodiazepines, being a major class of compounds used for treatment of anxiety present a narrow margin of safety between the anxiolytic effect and unwanted side effects (Nitesh et al., 2012). Melanthera scandens, belonging to the Asteraceae family, is a scandent annual or perennial herb up to 4 m high that is widely distributed across tropical Africa. The infusion of leaves is used as an emetic, cough and febrile headache medicine. In Côte d’Ivoire, the leaves are used as a purgative and an antidote against poisoning (Affia et al., 2011).In Bushenyi, western Uganda, infusion of the leaves is used among others in the management of seizures in addition to being used to clean teeth. The crude leaf extract of M. scandens has been reported to contain anti-inflammatory and analgesic activities (Jude et al., 2012). Despite the fact that M. scandens is well known to possess interesting properties in traditional medicine it has not been studied for its anxiolytic and anticonvulsant activities. This study was aimed at providing experimental support for the traditional medicinal use of the leaf water and ethanolic extracts of M. scandens in the management of epilepsy as well as anxiety. We hypothesized that the leaf aqueous and ethanolic extracts of M. scandens are effective in prevention of PTZ induced convulsions and have anxiolytic activity in rats.
This current study was conducted to determine the anticonvulsant and anxiolytic activity of the leaf water and ethanolic extracts of M. scandens.
Plant materials and extraction
The whole plant was collected in April 2014 from a bush in Nyakabirizi, Bushenyi district, Western Uganda. The, plant M. scandens, was authenticated by Dr. Eunice Olet, a Botanist from the Department of Biology, Mbarara University of Science and Technology (MUST), Uganda and a Voucher number (Silvano Twinomujuni 001) was kept in the herbarium for reference. Extraction was done according to Sutapa et al. (2012) with modifications in which the fresh plant leaves were washed and shade dried for two weeks and then ground. The powder (300 g) was dissolved in 2 L of distilled water or 2 L of 95% ethanol at room temperature, with intermittent shaking for 24 h, filtered using a filter paper to obtain water and ethanol extracts respectively. The liquid aqueous filtrate was evaporated to dryness in an oven at 60°C over 4 days while the ethanolic extract was dried at 40°C over 3 days. The dried crude extracts were stored in a refrigerator at 4°C until use for the proposed experiment. The yield of ethanol extract and water extract were11.9% (39.6 g/300 g) and 17.8% (53.5 g/300 g) of dry weight respectively.
Chemicals and drugs
PTZ was obtained from Sigma (USA); ethanol was procured from Scharlab S.L (Spain); diazepam injection was procured from Gland Pharma Ltd, India. Prior to use, all drugs/chemicals were freshly prepared in distilled water to the desired concentration.
Animals
Male Wistar rats (120 to 200 g) used in this study were obtained from the animal house facility of the Department of Pharmacology, MUST. They were maintained on a 12 h on and 12 h off light/dark schedule with free access to food and water, except during experimental procedures when they were fasted for 12 h before the experiment. All procedures involving animals were conducted in accordance with the Guidelines for the Humane Care and Use of Laboratory Animals published by National Institutes of Health, United States (Zandieh et al., 2010; OECD, 2000). The Institutional Review Board of Mbarara University approved the research. All laboratory experiments were conducted between 9:00 and 17:00 h. Animals were grouped in five groups of 8 animals each for each type of test conducted.
Phytochemical screening
Extracts of the dry powdered leaves of M. scandens were analyzed for the presence of various phytochemicals like alkaloids, terpenoids, flavonoids, phytosterols, proteins, reducing sugars, glycosides, phenols, tannins, saponins, free aminoacids and arginine using standard phytochemical analysis procedures specified by Trease and Evans (2012).
Elevated plus maze test
The elevated plus maze that was used in this study is the one described by Alicia and Cheryl (2007). The plus maze consists of two opposite open arms, 50 cm long and 10 cm wide, crossed with two closed arms of the same dimensions with 30 cm-high walls.
The arms are connected with a central square, 7.5 cm × 7.5 cm, to give the apparatus the shape of a plus sign. The whole apparatus was placed on an even floor to avoid unnecessary movements. Study animals were put into eight groups each containing 8 animals (n=8) and the following treatments were administered per group: Group I was treated with 250 mg/kg water extract (WE); group II 500 mg WE; group III 1000 mg WE; group IV 250 mg ethanolic extract (EE); group V 500mg EE; group VI 1000 mg EE; group VII 3 mg/kg Diazepam while the group VIII was treated with distilled water. 60 min after oral treatment with the extracts, each animal was placed individually in the center of the maze, facing the closed arm, after which the number of entries and time spent in the enclosed and open arms was recorded during the next five minutes using a video tracking system. Animals, which are anxious, are expected to spend more time in the closed arms while animals, which are not anxious, make more entries into and spend more time in the open arms. An arm entry was defined as the presence of all four feet in that particular arm. The maze was cleaned after each trial to remove any residue or odor of the animals. After the elevated plus maze test, the animals were returned to the cages to be used for anticonvulsant activity test.
Pentylenetetrazol (PTZ) induced seizures
Two days after elevated plus maze test, the same animals were orally treated with the extracts as follows: Group I was treated with 250 mg/kg water extract (WE); group II 500 mg/kg WE; group III 1000 mg /kg WE; group IV 250 mg/kg ethanol extract (EE); group V 500 mg/kg EE; group VI 1000 mg/kg EE; group VII 5 mg/kg diazepam (positive control) while the group VIII was treated with distilled water. Doses above were chosen basing on the results of acute toxicity test and the need to compare the activity for similar dose levels for the two extracts. The LD50 for the ethanol extract was estimated at 6.708 g/kg however the water extract was found safe up to 9.0 g/kg.
After 60 min, PTZ (60 mg/kg, i.p) was administered to all the groups. Each animal was individually placed in glass cage and observed for convulsive behavior for 30 min. The time of seizure onset, seizure duration and seizure behavior score (seizure severity) were recorded. Grading of seizure severity was done using a scoring system according to Alele and Rujumba (2011) as follows: Grade 0: no signs of motor seizure activity during the 30 min observation period; Grade 1: staring, mouth or facial movements; Grade 2: head nodding or isolated twitches; Grade 3: unilateral/bilateral forelimb clonus; Grade 4: rearing; Grade 5: loss of posture, jumping; Grade 6: clonic/tonic seizures; Grade 7: full tonic; Grade 8: death.
Statistical analysis
Values for seizure latency, duration, severity time spent and entries into the open and closed arms of the plus maze were statistically analyzed by two-way analysis of variance (ANOVA) followed by multiple comparison tests. Comparison between controls and test groups was performed by Bonferroni, Tukey's and Sidak’s post hoc tests using GraphPad Prism version 6.0. Data shown are mean ±Standard error of mean (SEM) for 8 rats per group. P values less than 0.05 (P<0.05) were taken to be the c criterion for statistical significance.
Phytochemical screening
Phytochemical screening revealed the presence, in both extracts, of phytosterols, proteins, reducing sugars, glycosides, carbohydrate, tannins, phenols, saponins, free amino acids and Arginine except flavonoids which were present only in the water extract (Table 1).
PTZ induced seizures
There was a significant increase in the time taken to see the first signs of PTZ induced convulsions with MS WE at 500 mg/kg compared to distilled water while there was no significant effect on the time taken for seizure onset in the MS EE treated rats compared to distilled water (Table 2). Both MS WE and MS EE did not have any significant effect on seizure duration (Table 3).
The seizure severity score was decreased significantly for both MS WE and MS EE at a dose of 1000 mg/kg (Table 4). Animals that were treated with Diazepam (5 mg/kg), the positive control, did not show any signs of seizure activity.
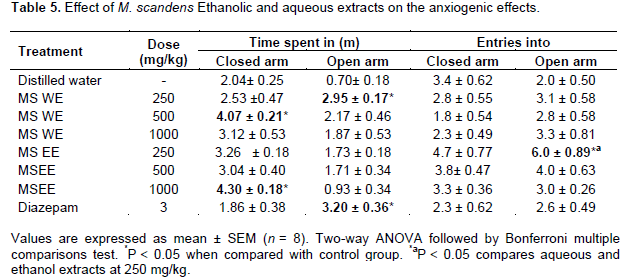
Effects of MS WE and MS EE on elevated plus maze test
In this test, the number of entries and time spent in the open arms were considered for the analysis of anxiolytic activity and the total number of entries in both the arms (enclosed and open arms) was considered for the evaluation of locomotor activity of animals (Varsha and Patel, 2010). MS WE and MSEE at the lowest dose of 250 mg/kg significantly increased the time spent in the open arm and increased entries into the open arm respectively compared to distilled water. At higher doses (500 and 1000 mg/kg), both extracts did not significantly increase the number of entries or time spent in the open arms. The total time spent in the closed arms was significantly increased at a dose of 1000 mg/kg (MS EE) and 500 mg/kg (MS WE) compared to distilled water. Animals treated with MS EE spent more time in the open arms compared to those treated with MS WE at 250 mg/kg, indicating that the MS EE had better anxiolytic activity than MS WE. Diazepam (3 mg/kg, i.p.), the positive control, significantly increased the time spent in the open arms (Table 5).
Phytochemical screening revealed the presence, in both extracts, of phytosterols, proteins, reducing sugars, glycosides, carbohydrate, tannins, phenols, saponins, free amino acids and arginine except flavonoids which were present only in the water extract. These findings are in agreement with the findings by Omoyeni et al. (2012); Fagbohun et al. (2012); Okokon et al. (2012) and Ndam et al. (2014). However, we did not find alkaloids and terpenoids, which were not found in the studies cited above.
Our findings demonstrated that M. scandens leaf extracts have anticonvulsant effects on PTZ model of epilepsy in rats. MS WE at a dose of 500 mg/kg increased seizure latency, while both MS WE and MS EE significantly reduced the severity of seizures. Pretreatment with M. scandens extracts protected the animals against PTZ induced death seizures with the percentage of seizure protection highest at 1000 mg/kg (Table 2). The medicinal value of plants lies in some chemical substances (phytochemicals) that have a definite physiological action on the human body (Amin et al., 2013; Datta et al., 2003; Dubois et al., 1986). The observed anticonvulsant activity in this study can be attributed to M. scandens extracts.
PTZ exerts its convulsant effects by inhibiting the activity of gamma amino butyric acid (GABA) at GABA-A receptors (DeSarro et al., 1999). GABA is a major inhibitory neurotransmitter, which is implicated in epilepsy. The enhancement of GABA neurotransmission attenuates convulsions while inhibition of the neuro-transmission of GABA enhances convulsions (Hoang and Hai, 2014). Diazepam is a known conventional antiepileptic agent that generally inhibits sodium currents and enhances GABA transmission. As expected, diazepam (5 mg/kg, i.p.) pretreated rats did not have any convulsive episode or show any mortality when treated with PTZ.
Since the extracts showed anticonvulsant effect against PTZ induced seizures, it is probable that they may be interfering with GABA transmission to exert their anticonvulsant effect. This is in agreement with findings of studies carried out by Hui et al., 2014 and Paramdeep et al., 2014, who found out that alkaloids, flavonoids, terpenoids, saponins, and coumarins enhance GABA transmission. Therefore, flavonoids and saponins may be responsible for the anticonvulsant activity observed in this study.
The elevated plus maze is considered to be an etiologically valid animal model of anxiety. The number of entries and time spent in the open arms have been found to be increased by anxiolytics and reduced by anxiogenic agents (Pellow et al., 1985). Both MS WE and MS EE showed anxiolytic activity at a lower dose of 250 mg/kg however, such activity was not observed at higher doses (500 and 1000 mg/kg) compared to the control. Animals spent more time in the closed arms and made fewer entries into the open arms compared to the control, at higher doses, as locomotor activity could have been impaired following after M. scandens extract administration. Available literature reports describe the action of benzodiazepines, such as diazepam, as anxiolytics (at low doses) and as anticonvulsants, also producing sedation and myorelaxant effects at higher doses (Wolffgramm et al., 1994). Reduction in the locomotor activity by Both MS WE and MS EE in the elevated plus maze test may be correlated with central nervous depression. Diazepam reduced the animal's natural aversion to the open arms and maze exploration. This was probably because the dose of diazepam used in this study (3 mg/kg) was higher than that of Varsha and Patel (2010) (1 mg/kg) who found out that diazepam increased the animal's natural aversion to the open arms and promoted maze exploration.
In various studies, (Sandeep and Suresh, 2010; Herrera et al., 2008), flavonoids have been shown to have antianxiety activity. The anxiolytic effect of flavonoids has been attributed to its effect on benzodiazepine receptors and central nervous system (Sandeep and Suresh, 2010). Therefore, flavonoids may be responsible for the anti-anxiety activity observed in this study. This study provides experimental support for the traditional medicinal use of this plant for the management of epilepsy and anxiety.
The authors have declared no conflict of interests.
The project described was supported by the MESAU-MEPI programmatic Award through Award Number 1R24TW008886 from the Fogarty International Center. The content is solely the responsibility of the authors and does not necessarily represent the views of the Fogarty International Center or the National Institute of Health. We would like to thank the Review and Ethics Committee of Mbarara University of Science and Technology for the guidance they gave us while carrying out this study. The authors also gratefully thank David Nkwangu, Hannifah Nantongo and Martin Amanya for their contribution in this study.
REFERENCES
|
Affia BF, Tonzibo ZF, Koffi AM, Chalard P, Figueredo G (2011). Chemical Composition of Essential Oil of Melanthera scandens (Schum. et Thonn.) Roberty. World Appl. Sci. J. 15(7):992-995.
|
|
|
|
Alele PE, Rujumba JB (2011). Khat (Catha edulis) and ethanol co-dependence modulate seizure expression in a pentylenetetrazol seizure model. J. Ethnopharmacol. 137(3):1431-1436.
Crossref
|
|
|
|
|
Alicia AW, Cheryl AF (2007). The use of the elevated plus maze as an assay of anxiety-related behavior in rodents. Nat. Protoc. 2(2):322-328.
Crossref
|
|
|
|
|
Amin MM, Sawhney SS, Jassal MMS (2013). Qualitative and quantitative analysis of phytochemicals of Taraxacum officinale. Wudpecker J. Pharm. Pharmocol. 2(1):001-005.
|
|
|
|
|
Datta BK, Datta SK, Chowdhury MM, Khan TH, Kundu JK, Rashid MA, Deckers CL, Genton P, Sills GJ, Schmidt D (2003). Current limitations of antiepileptic drug therapy: a conference review. Epilepsy Res. 53:1-17.
Crossref
|
|
|
|
|
DeSarro A, Cecchetti V, Fravolini V, Naccari F, Tabarrini O, DeSarro G (1999). Effects of novel 6-desfluoroquinolones and classic quinolones on pentylenetetrazole-induced seizures in mice. Antimicrob. Agents Chemother. 43(7):1729-36.
|
|
|
|
|
Dubois M, Ilyas M, Wagner H (1986). Cussonosides A and B, two Triterpene saponins-Saponin from Cussonia bateri. Planta Med. 52(2):80-83.
Crossref
|
|
|
|
|
Fagbohun ED, Lawal OU, Ore ME (2012). The proximate, mineral and phytochemical analysis of the leaves of Ocimum gratissimum L., Melanthera scandens A. and Leea guineensis L. and their medicinal value. Int. J. Appl. Biol. Pharm. Technol. 3(1):15-22.
|
|
|
|
|
Herrera-Ruiz M, Román-Ramos R, Zamilpa A, Tortoriello J, Jiménez-Ferrer JE (2008). Flavonoids from Tilia americana with anxiolytic activity in plus-maze test. J. Ethnopharmacol. 118(2):312-317.
Crossref
|
|
|
|
|
Hoang LS, Phan THY (2014). Preliminary Phytochemical Screening, Acute Oral Toxicity and Anticonvulsant Activity of the Berries of Solanum nigrum Linn. Trop. J. Pharm. Res. 13(6):907-912.
Crossref
|
|
|
|
|
Jude EO, Ette OE, John AU, Jackson O (2012). Antiplasmodial and antiulcer activities of Melanthera scadens. Asian Pac. J. Trop. Biomed. pp. 16-20.
|
|
|
|
|
Kamalraj R (2011). Anticonvulsant Studies on Leaf Extract of Erythrina Indica Lam. Int. J. Pharm. Sci. Res. 2(10):2729-2732.
|
|
|
|
|
Muazu J, Kaita AH (2008). A Review of Traditional Plants Used in the Treatment of Epilepsy Amongst the Hausa/Fulani Tribes of Northern Nigeria. Afr. J. Tradit. Complement. Altern. Med. 5(4):387-390.
Crossref
|
|
|
|
|
Ndam LM, Mih AM, Fongod AGN, Tening AS, Tonjock RK, Enang JE, Hui-Ling Z, Jian-Bo W, Yi-Tao W, Bao-Cai L, Cheng X, Jing H, Peng L (2014). Medicinal compounds with antiepileptic/anticonvulsant activities. Epilepsia 55(1):3-16.
Crossref
|
|
|
|
|
Nitesh G, Manish G, Avninder SM, Bharphur SS, Sanjeev M, Sandeep GL (2012). Phytochemical studies and anti anxiey activity of uraria picta leaves. J. Pharm. Res. Opin. 2(5):39-40.
|
|
|
|
|
OECD (2000). Guidance Document on Acute Oral Toxicity. Environmental Health and Safety Monograph Series on Testing and Assessment No 24. Available at: http://www.oecd.org/chemicalsafety/testing/2765785.pdf
|
|
|
|
|
Okokon Jude E, Anwanga E Udoh, Samuel G Frank, Louis U Amazu (2012). Anti-inflammatory and analgesic activities of Melanthera scandens. Asian Pac J. Trop. Biomed. 2(2):144-148.
Crossref
|
|
|
|
|
Omoyeni OA, Aterigbade E, Akinyeye RO, Olowu RA (2012). Phytochemical screening, nutritional/anti-nutritional and amino acid compositions of Nigeria Melanthera Scandens. Sci. Rev. Chem. Commun. 2(1):20-30.
|
|
|
|
|
Paramdeep S, Damanpreet S, Rajesh KG (2014). Phytoflavonoids: antiepileptics for the future. Int. J. Pharm. Pharm. Sci. 6(8):51-66.
|
|
|
|
|
Pellow S, Chopin P, File SE, Briley M (1985). Validation of open, closed arm entries in an elevated plus-maze as a measure of anxiety in the rat. J. Neurosci. Methods 14:149-67.
Crossref
|
|
|
|
|
Sandeep G, Suresh K (2010). Anti-anxiety Activity Studies of Various Extracts of Pulsatilla nigricans Stoerck. Int. J. Pharm. Sci. Drug Res. 2(4):291-293.
|
|
|
|
|
Sridharamurthy NB, Muralidhar ST, Juganta DA, Channaveeraswamy THM (2013). Effect of fluoroquinolones for Anticonvulsant activities on PTZ induced seizures in mice. Int. J. Adv. Res. 1(8):34-45.
|
|
|
|
|
Surajit S, Goutam D, Nilotpal M, Ananda RG, Tusharkanti G (2012). Anticonvulsant effect of Marsilea quadrifolia Linn.on pentylenetetrazole induced seizure: A behavioral and EEG study in rats. J. Ethnopharmacol. 141:537-541.
Crossref
|
|
|
|
|
Sutapa D, Rana D, Subhangkar N (2012). Phytochemical screening and evaluation of anti-inflammatory activity of methanolic extract of Abroma augusta Linn. Asian Pac. J. Trop. Dis. S114-S117.
|
|
|
|
|
Varsha JG, Bharatkumar GP (2010). Effect of hydroalcoholic extract of Sphaeranthus indicus against experimentally induced anxiety, depression and convulsions in rodents. Int. J. Ayurveda Res. 1(2):87-92.
Crossref
|
|
|
|
|
Wolffgramm J, Mikolaiczyk C, Coper H (1994). Acute and subchronic benzodiazepine-barbiturate-interations on behaviour and physiological responses of the mouse.Naunyn-Schmiedeberg's. Arch. Pharmacol. 349:279-86.
Crossref
|
|
|
|
|
Zandieh FM, Alireza H, Basira Z, Omid K Ahmad RD (2010). Anticonvulsant effect of celecoxib on pentylenetetrazole induced convulsion: modulation by NO pathway Department of Pharmacology. Acta Neurobiol. Exp. (Wars). 70(4):390-397.
|
|