Full Length Research Paper
ABSTRACT
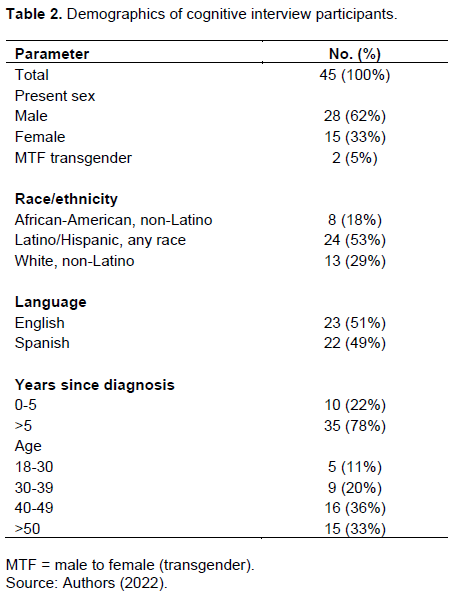
Intimate partner violence (IPV) is a significant and under-reported health problem. Legacy measures of IPV lack brevity and/or are relevant only to specific populations, which limit their usefulness for routine clinical care. We developed a brief patient-reported screening instrument of past-year intimate partner violence (IPV). We developed an item pool from validated IPV screening instruments, dimensionalized and winnowed its content to select candidate items. We conducted interviews with English and Spanish-speaking persons in HIV care in six U.S. primary care clinics to assess their comprehensibility, which informed the development of the four-item instrument (IPV-4). After integration into care we performed chart review for indication of IPV in the past 5 years to assess impact. We identified 68 items from 12 instruments and winnowed content within dimensions of physical, sexual, and psychological violence. We then presented 11 candidate items to PWH in interviews (n=45, 49% Spanish-language; mean age 45 years; 62% cisgender male, 33% cisgender female, 5% transgender female; 71% nonwhite). The resulting instrument was well-understood in English and Spanish and relevant across gender and sexual orientation. PWH (n=6415) completed the IPV-4 in clinical care settings; 9% reported any type of IPV and 5% reported physical and/or sexual violence. In chart notes of a single-site subset of PWH (n=1756), of those indicating physical and/or sexual violence on the IPV-4 with medical records available from the past five years (n=63), only 19% of PWH had prior notes indicating IPV in that time period. The IPV-4 is a brief, gender/sexual orientation-neutral, clinically relevant screening instrumentthat identifies and dimensionalizes past-year IPV present in 9% of PWH in routine care.
Key words: HIV care, intimate partner violence, patient-reported outcome measures.
INTRODUCTION
Intimate partner violence (IPV) is a significant and under-reported public health problem with a lifetime prevalence of 1 in 5 women and 1 in 7 men having experienced severe physical violence (Centers for Disease Control, 2021b; Huecker et al., 2022; Morgan, 2021). IPV refers to “physical violence, sexual violence, stalking and psychological aggression by a current or former intimate partner” (Centers for Disease Control, 2021a). An “intimate partner” is defined as a current or former dating partner or spouse (Centers for Disease Control, 2021b). Lifelong consequences of IPV beyond injury and death include poor physical and mental health outcomes, as well as substance abuse (Centers for Disease Control, 2021b).
The prevalence of IPV among PWH in the U.S. is estimated to be higher than that reported for the general population. A national survey found 26% of PWH reported ever having experienced IPV, with 4% reporting IPV in the past 12 months. Rates of 12-month IPV were similar between those who identify as cisgender men or women (4.4 vs 4.5% respectively), with transgender-identified PWH reporting a higher rate at 7.7% (Lemons-Lyn et al., 2021). By sexual orientation, bisexual and heterosexual women with HIV showed the highest lifetime rates (52 and 35%, respectively), followed by gay men (28%); while current 12-month rates were highest among bisexual women and men, followed by gay men (15, 8, and 5%, respectively) (Lemons-Lyn et al., 2021).
IPV may be particularly common among PWH who use illicit drugs: one study found very high rates among female crack cocaine users (68%) and also among gay and bisexual men and transgender PWH (71%) (Kalokhe et al., 2012). IPV has also been associated with increased health care utilization and health care costs among sexual minority men (O'Cleirigh et al., 2018) and women (Valentine et al., 2015) and HIV status among sexual minority men (O'Cleirigh et al., 2018). Among cisgender male and female PWH, IPV has been associated with a negative impact on viral suppression (Fredericksen et al., 2021a; Hatcher et al., 2015), ARV adherence(Fredericksen et al., 2021a; Pantalone et al., 2018), substance use (Fredericksen et al., 2021), retention in care (Hatcher et al., 2015; Kalokhe et al., 2012; Pantalone et al.,), depression (Fredericksen, 2021a),and HIV transmission risk behavior (Harkness et al., 2019; Kalokhe et al., 2012). IPV has also been associated with sexual risk for HIV among black MSM(Williams et al., 2015). Psychological violence, even in the absence of physical or sexual violence, has been associated with depression, substance use, and poor virologic outcomes among people with HIV (Fredericksen, Nance, et al., 2021a). These relationships underscore the importance of improving the availability and uptake of quality IPV screening and assessment to support health outcomes in community and primary care settings.
IPV is both under-addressed and inadequately addressed in clinical care (Morse et al., 2012; Perone et al., 2022) likely in part due to barriers such as lack of provider training to effectively respond to IPV, lack of time, and lack of effective interventions (Kalra et al., 2021; Sprague et al., 2012). The use of IPV screening questionnaires is known to increase IPV identification (O'Doherty et al., 2014). Screening using an assessment of same-day electronic tablet-based patient-reported outcome measures (PROs) may greatly assist providers in identifying IPV. Tablet-based approaches are known to reduce social desirability bias (Adebajo et al., 2014) and significantly increase provider awareness for other difficult-to-disclose symptoms and behaviors such as depression, substance use, and inadequate medication adherence(Crane et al., 2017). Clinical assessments of PROs have been well-tolerated by patients and useful to providers (Fredericksen, Harding, et al., 2021b; Fredericksen et al., 2016; Jones et al., 2014; Sharma et al., 2016; Short et al., 2022; Stover et al., 2015).
While no “gold standard” exists for IPV measurement in clinical care settings for routine screening, multiple agencies including the World Health Organization have indicated best practices such as the use of a clear timeframe and inquiry into specific partner behaviors (Yount et al., 2022). Many legacy IPV measures were developed specifically for cisgender heterosexual female respondents, and/or use male pronouns to presume the perpetrator (Brown et al., 2000; Campbell, 1986; Glass et al., 2001; McFarlane et al., 1995; Smith et al., 1995). Inaddition, many IPV measures are lengthy, limiting the feasibility of their use in routine clinical care (Fitzsimmons, 2019 a). We developed a brief gender and sexual orientation-neutral brief IPV instrument to screen for IPV in clinical HIV care and other settings, based on literature and legacy item review and patient feedback.
We implemented the scale in six primary HIV care clinics.
METHODOLOGY
Item pool development, categorization, and winnowing
In concordance with NIH-Patient Reported Outcomes Measurement Information System (PROMIS) protocols for instrument development (Cella et al., 2007), we developed an item pool of legacy IPV items based on literature review. We solicited assistance of health reference librarians to identify IPV measures developed or used in care since 1980. Our initial search included terms “intimate partner violence”, “domestic violence”, or “partner violence” and “screening” yielding 827 citations in PubMed. We scanned citations, excluding instruments from population-based surveys not intended for clinical care, instruments not in North American English or Spanish, instruments requiring interviewer administration, instruments not known to be used in clinical care and lacking evidence of reliability or validity testing, instruments based on something other than text (e.g., marking bodily harm on body maps), and instruments our team could not access after two attempts to contact authors. Two qualitative researchers (RF, EF) independently categorized candidate items using an open-coding process and achieved consensus on final fixed codes. Three reviewers independently (RF, EF, SB) winnowed items into a smaller pool, selecting the best among alternatives with similar content, using the PROMIS Qualitative Item Review (QIR) process (DeWalt et al., 2007). We reconciled discordance in QIR coding through group discussion (RF, EF, SB).
Cognitive interview study population and recruitment
All PWH over age 18 and willing/able to consent were eligible for participation in the cognitive interview. We recruited PWH at four U.S. clinics within the Centers for AIDS Research Network of Integrated Clinical Systems (CNICS): Fenway Community Health- Boston, MA; 1917 Clinic at the University of Alabama-Birmingham; Owen Clinic at the University of California at San Diego; and Madison Clinic at Harborview Medical Center/University of Washington-Seattle. We informed patients of their eligibility on-site while waiting for their scheduled provider visit. Human subject committees at each site approved all research activity.
Cognitive interview testing
We tested candidate items for comprehensibility among English-and Spanish-speaking PWH in their respective languages. Interviews were approximately 45 min; participants received $25 compensation. We calculated the proportion of patients that comprehended each item and reviewed all items that were less- than-unanimously understood for opportunities to clarify.
Final development of IPV-4
We created the final version of the IPV-4 based on universal comprehensibility of items. During development, we faced the question of what aspects of IPV are most clinically relevant to identify, and in doing so, considered item content that a) threatened the patient’s short-and long-term safety/well-being, and b) was not prone to misinterpretation, yielding ‘false positive’ results. With a focus on brevity to foster feasibility in clinical care settings, we selected one item to represent each dimension for physical and sexual violence, and two that represented distinct aspects of psychological violence: one for unwanted feelings of being trapped/controlled by a partner, and the other for fearing being harmed by a partner.
Analysis of value added to care
We integrated the IPV-4 into clinical care at the 4 cognitive interview sites, as well as two additional sites (Ward 86 at University of California-San Francisco/Zuckerberg Hospital, and University of North Carolina), as part of a routine ~10-min comprehensive clinical assessment of patient-reported outcomes (PROs) including depression, substance use, adherence, and others self-administered by patients on-site prior to seeing their providers. The CNICS clinical assessment of PROs has been fully described elsewhere (Crane et al., 2007; Fredericksen et al., 2012). If patients indicated physical or sexual IPV in the assessment, automated pager alerts notified health care team members in real time. Providers were notified of any indication of violence (including psychological) by receiving summarized assessment results immediately prior to seeing the patient.
Selecting one CNICS site (UW), we identified the proportion of PWH reporting IPV overall and by IPV type using dates 6/6/16 through 11/6/19. We sought to better understand the impact that identification of IPV may have had on patient care by performing a chart review analysis. The objective was to determine the extent to which IPV identified by the IPV-4 was likely already known to providers or was adding new information. At this site, among all individuals who indicated IPV on the IPV-4, we examined medical record documentation 5 years prior to indication. Specifically, we examined documentation for any prior mention of IPV in outpatient chart notes from primary care, psychiatrists, psychologists, social work/case managers, and emergency department visit notes, dating back 5 years from the date IPV was indicated on the IPV-4. We tracked whether any sexual, physical, or threatening IPV was identified in the chart notes, and whether an intervention or plan was made.
RESULTS
Item pool development, categorization, winnowing, and selection for cognitive interviews
We identified 68 items from 12 instruments for three IPV dimensions: psychological, physical, and sexual violence. We further subdivided codes of psychological violence into two categories: unwanted attempts by a partner to assert control over the patient’s actions, and partner behavior that incites patients’ fear for their safety. In some cases, we combined items that were similar to more fully describe the concept; for example, in the case of physical violence, we combined items describing impact (e.g., hit/kick/punch) rather than asking these separately. Winnowing resulted in a pool of 11 distinct legacy and adapted legacy candidate items with representation across all dimensions. To minimize patients’ burden, we formatted items to conform to a ‘yes/no’ response option. The items were extracted from the following IPV instruments: Constructs of IPV for Gay and Bisexual Men (Stephenson et al., 2013), Fenway Community Health IPV Measure, Danger Assessment (Campbell, 1986; Campbell et al., 2009), Humiliation, Afraid, Rape, Kick (HARK)(Sohal et al., 2007), Hurt, Insult, Threaten, and Scream (HITS) (Sherin et al., 1998), Ongoing Abuse Screen (Ernst et al., 2002), and the Women Abuse Screening Tool (WAST) (Brown et al., 2000). Table 1 shows candidate cognitive interview items, their origins, and the IPV dimension each represents.
Cognitive interviews
We interviewed 23 English-speaking and 22 Spanish-speaking PWH (Table 2). Of the latter, 5 interviews were conducted as secondary interviews testing comprehensibility of slightly revised Spanish items.
Cognitive interviews
Cognitive interview results are organized by dimension.
Physical violence: The sole composite physical violence item, which assesses whether a partner “hit, kicked, punched, slapped, shoved, or otherwise physically hurt” the patient, was clearly understood by all English-speaking patients. Among Spanish speakers, however, some of these verbs were experienced as redundant. On the advice of native-Spanish speaking patients and team members, the Spanish version of the item was changed to use fewer verbs (“lo/a golpeó, pateó, o lastimó físicamente de alguna forma,” excluding the specific verbs for punch, slap, and shove) while still covering the English versions of the concepts.
Sexual violence: We tested two separate sexual; violence items: one querying sexual abuse by a partner the other asking whether a partner “pressured or forced you to do something sexual that you did not want to do”.
The former was poorly understood by patients, who found the item too broad (“What counts as sexual? What counts as abuse?”). Patients unanimously found the latter item clearer. Some noted its superior ability to distinguish between unwanted sexual activity and, for example, sexual play that could include consensual sado-masochistic elements (e.g., bondage).
(3) Psychological violence
(a) Partner “control”): Of the eight psychological violence items tested, four concerned the concept of being controlled by a partner. These included (1) controlling “where you go, who you talk to, or how you spend your
money”; (2) preventing the patient from communicating with or seeing friends/family/co-workers; (3) demanding and monitoring access to cell phone, email, social networking sites, finances or spending; and 4) being made to feel “isolated, trapped or like you were walking on eggshells in the relationship”. Patients found that the first item failed to consider whether the person had consented to the control, e.g., in the case of wanting their partner to control their finances, or when being cared for by a partner in the event of illness/disability. The second item, while unanimously understood, was felt to exclude important individuals, such as religious leaders and social workers. For the third item, the verb “monitor” was not believed to be necessarily invasive or abusive. The fourth item contained an English-specific expression (“walking on eggshells”) without a directly translatable Spanish-language equivalent, and the term “isolation” which was not universally understood.
To address patients’ concerns and improve comprehension, we crafted a composite “control” item, querying whether they felt “cut off from others, trapped, or controlled [by a partner] in a way you did not like”. The specification of “a way you did not like” was believed by patients to be key to identifying IPV; this distinction had been missing from many of the legacy items assessing partner ‘control’. We chose the term “cut off from others” as it simplified the potentially cumbersome alternative of reviewing specific types of contacts (e.g., friends, co-workers). This simplification maximized relevance to patients while maintaining fidelity to the concept of partner-controlled isolation. We chose the term “trapped” as it was well-understood in Spanish and English and distinct from the concept of being “cut off” from others, and to capture patients that might not be isolated socially but feel “trapped” unwillingly by their partners in any other sense.
(b) Being “made to feel afraid” by partner: Four items pertained to a partner provoking fear by screaming, yelling/cursing, or threatening harm against them. Some patients felt that being “screamed, yelled, or cursed” at was not always necessarily an indication of abuse. Being made to feel afraid was viewed as more concerning and specific to what was intended by the ‘screaming/yelling/cursing’ at. This prompted us to create the composite item querying whether a partner “made you feel afraid that they might try to hurt you in some way”.
(c) Humiliation and emotional abuse: An item querying “humiliation and emotional abuse” was poorly understood by patients due to the lack of a clear agreement or understanding regarding the meaning of both concepts. For example, a partner’s actions may not necessarily have been intended to humiliate the patient; or humiliation may have arisen from jealousy of the partner. The concept of “emotional abuse” as a general term was also problematic; patients were unclear regarding its definition and scope. Moreover, we were concerned that “emotional abuse” may capture patients without truly abusive partners, such as patients who feel at times emotionally hurt by the partner’s neglect or objectively non-abusive actions (e.g., spending time with friends the patient does not like). Given the ambiguity and need to narrowly define this term, which would likely require administering more than one additional item, and lack of superior or suitable alternatives for these concepts in the item pool, we opted to omit this item.
Final screening instrument
The final screening instrument (Figure 1) clearly defines “intimate partner” and is inclusive of several past and current partner types. We did not include persons with whom one has ongoing contact but lacks the emotional and/or physical intimacy shared by a romantic, domestic, or sexual partner. Patients described the importance of a longer recall period, noting that IPV may be sporadic; we thus selected a one-year period. In the interest of brevity and patient tolerability of the instrument, we selected one item each to represent physical and sexual violence, and two to represent separate aspects of psychological violence (being controlled/trapped and being made to feel afraid).
All concepts were present in both languages, and neither language lacked a concept found in the other. Differences were primarily semantic; items translated into Spanish maintained fidelity to their English-language concepts, even after minor alterations to wording.
Identification of IPV across all 6 CNICS sites
Of n=6415 patients administered the IPV-4 between 6/16/16 and 11/6/19, 594 (9%) indicated any IPV. Of these, 295 (5%) indicated physical IPV, sexual IPV, or both in the past year (216 or 3% indicated physical IPV, 180 or 3% indicated sexual IPV, and 101 or 2% indicated both). Two hundred ninety-one reported fearing harm from a partner (5%), and 479 reported feeling “trapped, cut off, or controlled in a way I did not like” (7%). The IPV-4 took on average 26 s to complete (maximum time 74 s).
Chart review analysis
Of n=1756 patients that were administered the IPV instrument as part of the clinical assessment of PROs in clinical care at UW between 6/16/16 and 11/6/19, we identified 158 PWH (9%) who indicated physical and/or sexual IPV via the IPV-4. Of these, 63 (40%) had been in care for their HIV at UW for ³5 years. We reviewed medical records for these 63 individuals, with an average of 34 visits per patient. Of these, only 12 (19%) had indications in medical records of any form of IPV up to five years prior to the date of indicating IPV on the IPV-4. This suggests that among PWH well known to their primary care delivery team, the IPV-4 may identify additional patients experiencing IPV than had previously been documented by their primary care providers or anyone else in the UW medical system.
DISCUSSION
We developed a 4-item screening instrument of physical, sexual, and psychological IPV in English and Spanish that addresses the need for a brief, gender-and sexual orientation-neutral assessment of IPV. The instrument was well- understood and well-tolerated by PWH. The IPV-4 includes specific focus on psychological violence, which among PWH and others is increasingly recognized as a factor associated with immune function and healthy behaviors (Fitzsimmons et al., 2019b; Jewkes et al., 2015; Kalokhe et al., 2016). We identified a 9% indication of IPV among PWH across CNICS sites, and, per chart reviewanalysis, identified substantially more IPV than had been previously identified by providers.
Our literature review confirmed a lack of consensus on a single well-validated patient-reported IPV screening instrument. We found that many IPV screening instruments were developed for population research purposes, were too lengthy to be feasible for use in routine clinical care, or used population-specific language (e.g., pregnant persons). Psychological violence measures proved particularly problematic for some patients, at times perceived as not necessarily reflective of abuse (e.g., in the case of a partner “controlling one’s money”).
PROs intended for routine clinical care work best when they are brief, clinically relevant, and easy to understand (Fredericksen et al., 2016; Stover et al., 2015). In developing the IPV-4, we found opportunities to improve brevity by consolidating language to simplify items while maintaining fidelity to concepts. We found it pertinent to consolidate a single physical abuse item that lists a variety of impact types (e.g., shove, kick, punch) rather than assessing each type of impact separately, since all forms are clinically concerning. For psychological violence, which manifests in innumerable forms, we generalized concepts of unwanted “control” and “being made to feel afraid”, rather than querying what was controlled, or in what way the patient was made to feel afraid. This level of detail could be more appropriate for follow up in the context of patient-provider discussion.
Computer-based IPV screening has been found to detect more IPV than face-to-face interviews (Miller et al., 2022) and to be preferred by patients (El Morr and Layal, 2020). We recommend same-day pre-visit computerized IPV PRO screening on-site prior to the appointment, so that clinicians may respond in real time as needed (e.g., using alerts generated by the screening), as is currently practiced in CNICS sites (Fredericksen et al., 2021b). The IPV-4 is a brief, well-vetted multidimensional instrument suitable for screening IPV in busy clinical care settings. It identified PWH that had experienced IPV and detected incidence that might have otherwise been missed.
Strengths
We interviewed a diverse patient sample across race, sex/gender, sexual orientation, and geographic area, oversampling ethnic minorities and cisgender women.
LIMITATIONS
In order to avoid re-traumatization of PWH that had experienced IPV, we did not conduct concept elicitation interviews.
CONCLUSION
Item pool development, the QIR process, and bilingual patient cognitive interviews informed development of the IPV-4, a brief, clinically relevant, comprehensive, well-tolerated screening instrument for IPV that is gender/sexual orientation-neutral. The IPV-4 was easily integrated into HIV care and identified a high prevalence of unsuspected IPV among PWH, including those well-established in care.
CONFLICT OF INTERESTS
The authors have not declared any conflict of interests.
ACKNOWLEDGMENTS
We thank participating patients for their candor and insights, and site staff for their contribution to this work. This research was funded by the Patient Centered Outcomes Research Institute (PCORI) #SC14-1403-14081. Additional support: National Institutes of Alcohol Abuse and Alcoholism (NIAAA) at the National Institutes of Health [U24AA020801, U01AA020793 and U01AA020802] and the National Institute of Allergy and Infectious Diseases (NIAID) at the National Institutes of Health [CNICS R24 AI067039, UW CFAR NIAID Grant P30 AI027757; and UAB CFAR grant P30 AI027767]
REFERENCES
|
Adebajo S, Obianwu O, Eluwa G, Vu L, Oginni A, Tun W, Sheehy M, Ahonsi B, Bashorun A, Idogho O, Karlyn A (2014). Comparison of audio computer assisted self-interview and face-to-face interview methods in eliciting HIV-related risks among men who have sex with men and men who inject drugs in Nigeria. PLoS One 9(1):e81981. |
|
|
Brown JB, Lent B, Schmidt G, Sas G (2000). Application of the Woman Abuse Screening Tool (WAST) and WAST-short in the family practice setting. Journal of Family Practice 49(10):896-903. |
|
|
Campbell JC (1986). Nursing assessment for risk of homicide with battered women. Advances in Nursing Science 8(4):36-51. |
|
|
Campbell JC, Webster DW, Glass, N (2009). The danger assessment: validation of a lethality risk assessment instrument for intimate partner femicide. Journal of Interpersonal Violence 24(4):653-674. |
|
|
Cella D, Yount S, Rothrock N, Gershon R, Cook K, Reeve B, Ader D, Fries JF, Bruce B, Rose, M (2007). The Patient-Reported Outcomes |
|
|
Measurement Information System (PROMIS): progress of an NIH Roadmap cooperative group during its first two years. Med Care 45(5 Suppl 1):S3-S11. |
|
|
Centers for Disease Control (2021). Violence prevention: intimate partner violence. |
|
|
Centers for Disease Control (2021). Violence prevention: intimate partner violence fast facts. |
|
|
Crane HM, Crane K, Tufano JT, Ralston JD, Wilson IB, Brown TD, |
|
|
Davis TE, Smith LF, Lober WB, McReynolds J, Dhanireddy S, Harrington RD, Rodriguez CV, Nance RM, Delaney JA, Safren SA, Kitahata MM, Fredericksen RJ (2017). HIV provider documentation and actions following patient reports of at-risk behaviors and conditions when identified by a web-based point-of-care assessment. AIDS and Behavior 21(11):3111-3121. |
|
|
Crane HM, Lober W, Webster E, Harrington RD, Crane PK, Davis, TE, Kitahata MM (2007). Routine collection of patient-reported outcomes in an HIV clinic setting: the first 100 patients. Current HIV Research 5(1)109-118. |
|
|
DeWalt DA, Rothrock N, Yount S, Stone AA, Group PC (2007). Evaluation of item candidates: the PROMIS qualitative item review. Med Care 45(5 Suppl 1):S12-21. |
|
|
El Morr C, Layal M (2020). Effectiveness of ICT-based intimate partner violence interventions: a systematic review. BMC Public Health 20(1):1372. |
|
|
Ernst AA, Weiss SJ, Cham E, Marquez M (2002). Comparison of three instruments for assessing ongoing intimate partner violence. Medical Science Monitor 8(3):CR197-201. |
|
|
Fitzsimmons E, Loo S, Dougherty S, Mathews WC, Mugavero MJ, Mayer KH, Potter J, O'Cleirigh C, Crane PK, Crane HM, Fredericksen RJ (2019a). Development and content validation of a brief patient-reported measure of intimate partner violence for use in HIV care International Society for Quality of Life Research Annual Conference, San Diego, CA. |
|
|
Fitzsimmons E, Fredericksen RJ, Nance RM, Whitney BM, Harding BN, Del Rio C, Feaster DJ, Kalokhe AS, Mayer KH, Metsch LR, O'Cleirigh C, Smith L, Delaney JA, Crane HM (2019b). Impact and correlates of psychological intimate partner violence on antiretroviral adherence and clinical outcomes among patients in HIV care International Association of Physicians in AIDS Care, Miami Beach, FL. |
|
|
Fredericksen RJ, Crane P, Tufano J, Ralston J, Schmidt S, Brown T, D L, Harrington R, Dhanireddy S, Stone T, Lober W, Kitahata M, Crane H (2012). Integrating a web-based patient assessment into primary care for HIV-infected adults. Journal of AIDS and HIV Research 4(2):47. |
|
|
Fredericksen RJ, Nance RM, Whitney BM, Harding BN, Fitzsimmons E, Del Rio C, Eron J, Feaster DJ, Kalokhe AS, Mathews WC, Mayer KH, Metsch LR, Mugavero, MJ, Potter J, O'Cleirigh C, Napravnik S, Rodriguez B, Ruderman S, Jac D, Crane HM (2021a). Correlates of psychological intimate partner violence with HIV care outcomes on patients in HIV care. BMC Public Health 21(1):1824. |
|
|
Fredericksen RJ, Harding BN, Ruderman SA, McReynolds J, Barnes G, Lober WB, Fitzsimmons E, Nance RM, Whitney BM, Delaney JAC, Mathews WC, Willig J, Crane PK, Crane HM (2021b). Patient acceptability and usability of a self-administered electronic patient-reported outcome assessment in HIV care: relationship with health behaviors and outcomes. AIDS Care 33(9):1167-1177. |
|
|
Fredericksen RJ, Tufano J, Ralston J, McReynolds J, Stewart M, Lober WB, Mayer KH, Mathews WC, Mugavero MJ, Crane PK, Crane HM (2016). Provider perceptions of the value of same-day, electronic patient-reported measures for use in clinical HIV care AIDS Care 1-6. |
|
|
Glass N, Dearwater S, Campbell J (2001). Intimate partner violence screening and intervention: data from eleven Pennsylvania and California community hospital emergency departments. Journal of Emergency Nursing 27(2):141-149. |
|
|
Harkness A, Bainter SA, O'Cleirigh C, Albright C, Mayer KH, Safren SA (2019). Longitudinal effects of syndemics on HIV-positive sexual minority men's sexual health behaviors. Archives of Sexual Behavior 48(4):1159-1170. |
|
|
Hatcher AM, Smout EM, Turan JM, Christofides N, Stockl H (2015). Intimate partner violence and engagement in HIV care and treatment among women: a systematic review and meta-analysis. AIDS 29(16):2183-2194. |
|
|
Huecker MR, King KC, Jordan GA, Smock W (2022). Domestic Violence. In StatPearls. |
|
|
Jewkes R, Dunkle K, Jama-Shai N, Gray G (2015). Impact of exposure to intimate partner violence on CD4+ and CD8+ T cell decay in HIV infected women: longitudinal study. PLoS One 10(3):e0122001. |
|
|
Jones J, Stephenson R, Smith DK, Toledo L, La Pointe A, Taussig J, Sullivan PS (2014). Acceptability and willingness among men who have sex with men (MSM) to use a tablet-based HIV risk assessment in a clinical setting. Springerplus 3(1):1-7. |
|
|
Kalokhe AS, Ibegbu CC, Kaur SP, Amara RR, Kelley, ME, Del Rio C, Stephenson R (2016). Intimate partner violence Is associated with increased Cd4+ T-Cell activation among Hiv-negative high-risk women. Pathogens and Immunity 1(1):193-213. |
|
|
Kalokhe AS., Paranjape A, Bell CE, Cardenas GA, Kuper T, Metsch LR, Del Rio, C (2012). Intimate partner violence among HIV-infected crack cocaine users. AIDS Patient Care STDS 26(4):234-240. |
|
|
Kalra N, Hooker L, Reisenhofer S, Di Tanna GL, Garcia-Moreno C (2021). Training healthcare providers to respond to intimate partner violence against women. Cochrane Database of Systematic Reviews 5:CD012423. |
|
|
Lemons-Lyn AB, Baugher AR, Dasgupta S, Fagan JL, Smith SG, Shouse RL (202). Intimate Partner Violence Experienced by Adults With Diagnosed HIV in the U.S. American Journal of Preventive medicine 60(6):747-756. |
|
|
McFarlane J, Greenberg L, Weltge A, Watson M (1995). Identification of abuse in emergency departments: effectiveness of a two-question screening tool. Journal of Emergency Nursing 21(5):391-394. |
|
|
Miller DP Jr, Foley KL, Bundy R, Dharod A, Wright E, Dignan M, Snavely AC (2022). Universal Screening in Primary Care Practices by Self-administered Tablet vs Nursing Staff. JAMA Network Open, 5(3):e221480-e221480. |
|
|
Morgan RE, Thompson A (2021). Criminal victimization, 2020. Washington, DC: National Crime Victimization Survey, Bureau of Justice Statistics. |
|
|
Morse DS, Lafleur R, Fogarty CT, Mittal M, Cerulli C (2012). "They told me to leave": how health care providers address intimate partner violence. The Journal of the American Board of Family Medicine 25(3):333-342. |
|
|
O'Cleirigh C, Pantalone DW, Batchelder AW, Hatzenbuehler ML, Marquez SM, Grasso C, Mayer KH (2018). Co-occurring psychosocial problems predict HIV status and increased health care costs and utilization among sexual minority men. Journal of Behavioral Medicine 41(4):450-457. |
|
|
O'Doherty LJ, Taft A, Hegarty K, Ramsay J, Davidson LL, Feder G (2014). Screening women for intimate partner violence in healthcare settings: abridged Cochrane systematic review and meta-analysis. BMJ 348:g2913. |
|
|
Pantalone DW, Hessler DM, Simoni JM Mental health pathways from interpersonal violence to health-related outcomes in HIV-positive sexual minority men. Journal of Consulting And Clinical Psychology 78(3):387-397. |
|
|
Pantalone DW, Valentine SE, Woodward EN, O'Cleirigh C (2018). Syndemic indicators predict poor medication adherence and increased healthcare utilization for urban HIV-positive men who have sex with men. Journal of Gay and Lesbian Mental Health 22(1):71-87. |
|
|
Perone HR, Dietz NA, Belkowitz J, Bland S (2022). Intimate partner violence: analysis of current screening practices in the primary care setting. Family Practice 39(1):6-11. |
|
|
Sharma P, Dunn RL, Wei JT, Montie JE, Gilbert SM (2016). Evaluation of point-of-care PRO assessment in clinic settings: integration, parallel-forms reliability, and patient acceptability of electronic QOL measures during clinic visits. Quality of Life Research 25(3):575-583. |
|
|
Sherin KM, Sinacore JM, Li XQ, Zitter RE, Shakil A (1998). HITS: a short domestic violence screening tool for use in a family practice setting. Family Medicine-Kansas City 30:508-512. |
|
|
Short D, Fredericksen RJ, Crane HM, Fitzsimmons E, Suri S, Bacon J, Musten A, Gough K, Ramgopal M, Berry J, McReynolds J, Kroch A, Jacobs B, Hodge V, Korlipara D, Lober W (2022). Utility and Impact of the Implementation of Same-Day, Self-administered Electronic Patient-Reported Outcomes Assessments in Routine HIV Care in two North American Clinics. AIDS and Behavior 26(7):2409-2424. |
|
|
Siemieniuk RAC, Krentz HB, Miller P, Woodman K, Ko K, Gill, MJ (1999). The clinical implications of high rates of intimate partner violence against HIV-positive women. Journal of Acquired Immune Deficiency Syndromes 64(1):32-38. |
|
|
Siemieniuk RA, Miller P, Woodman K, Ko K, Krentz HB, Gill MJ (2013). Prevalence, clinical associations, and impact of intimate partner violence among HIV?infected gay and bisexual men: A population?based study. HIV Medicine 14(5):293-302. |
|
|
Smith PH, Tessaro I, Earp JA (1995). Women's experiences with battering: a conceptualization from qualitative research. Womens Health Issues 5(4):173-182. |
|
|
Sohal H, Eldridge S, Feder G (2007). The sensitivity and specificity of four questions (HARK) to identify intimate partner violence: a diagnostic accuracy study in general practice. BMC Family Practice 8(1):1-9. |
|
|
Sprague S, Madden K, Simunovic N, Godin K, Pham NK, Bhandari M, Goslings JC (2012). Barriers to screening for intimate partner violence. Women Health 52(6):587-605. |
|
|
Stephenson R, Hall CD, Williams W, Sato K, Finneran C (2013). Towards the development of an intimate partner violence screening tool for gay and bisexual men. Western Journal of Emergency Medicine 14(4):390-400. |
|
|
Stover A, Irwin DE, Chen RC, Chera BS, Mayer DK, Muss HB, Rosenstein DL, Shea TC, Wood WA, Lyons JC, Reeve BB (2015). Integrating patient-reported outcome measures into routine cancer care: cancer patients' and clinicians' perceptions of acceptability and value. Egems (Wash DC) 3(1):1169. |
|
|
Valentine, SE, Elsesser S, Grasso C, Safren SA, Bradford JB, Mereish E, O'Cleirigh C (2015). The Predictive Syndemic Effect of Multiple Psychosocial Problems on Health Care Costs and Utilization among Sexual Minority Women. Journal of Urban Health 92(6):1092-1104. |
|
|
Williams JK, Wilton L, Magnus M, Wang L, Wang J, Dyer TP, Koblin BA, Hucks-Ortiz C, Fields SD, Shoptaw S, Stephenson R, O'Cleirigh C, Cummings V, Team HIVPTNS (2015). Relation of Childhood Sexual Abuse, Intimate Partner Violence, and Depression to Risk Factors for HIV Among Black Men Who Have Sex With Men in 6 US Cities. American Journal of Public Health 105(12):2473-2481. |
|
|
Yount KM, Cheong YF, Khan Z, Bergenfeld I, Kaslow N, Clark CJ (2022). Global measurement of intimate partner violence to monitor Sustainable Development Goal 5. BMC Public Health 22(1):465. |
|
Copyright © 2024 Author(s) retain the copyright of this article.
This article is published under the terms of the Creative Commons Attribution License 4.0